Bone Health Risk Assessment
Your Bone Health Risk Assessment
As we get older, our skeleton isn’t as indestructible as it once seemed. Understanding how age weakens the frame can help you keep moving freely and avoid painful breaks. Below you’ll find the key facts you need to protect your bone health and stay active for years to come.
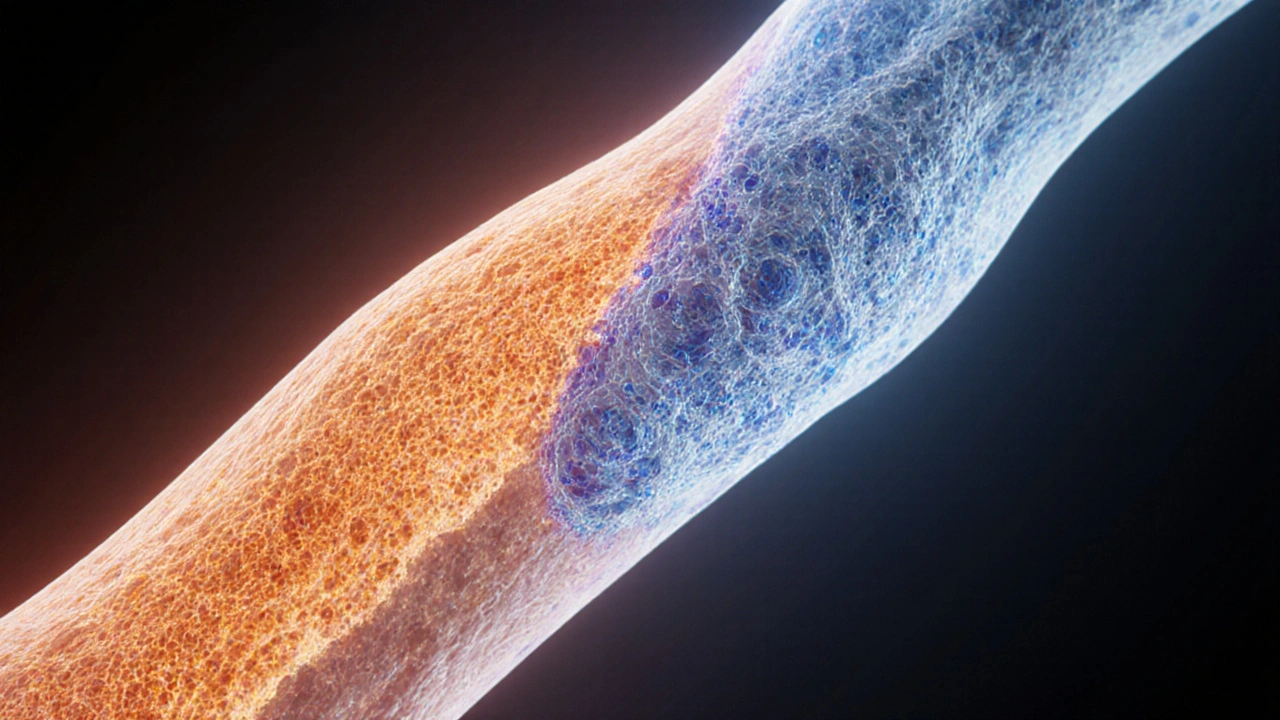
Why Bones Change with Age
When you’re young, Bone is a living tissue that constantly renews itself through a balanced cycle of breakdown and rebuilding. This process, known as bone remodeling, relies on two main cell types: osteoclasts that dissolve old bone, and osteoblasts that lay down new bone. In your twenties, the balance tips toward formation, allowing you to reach peak bone mass.
After the third decade, the remodeling balance gradually shifts. Bone resorption starts to outpace formation, leading to a slow loss of density. Hormonal changes-especially the drop in estrogen during menopause-speed up this decline for many women. Men also experience a gradual dip in testosterone, which can affect bone upkeep.
Common Types of Age‑Related Bone Damage
Osteoporosis is a condition characterized by reduced bone mass and structural deterioration, making bones fragile and more likely to fracture. It often goes unnoticed until a fracture occurs, typically in the hip, spine, or wrist.
Another frequent complaint is Osteoarthritis a degenerative joint disease where cartilage breaks down, leading to pain and reduced mobility. While not a direct loss of bone density, the altered joint mechanics can increase stress on surrounding bone, contributing to micro‑damage.
Even in the absence of these diseases, normal age‑related bone loss (sometimes called senile osteoporosis) can still raise fracture risk, especially when combined with poor nutrition or a sedentary lifestyle.
Key Nutrients that Keep Bones Strong
Two nutrients dominate the conversation: Calcium is the primary mineral that forms the hard matrix of bone and Vitamin D facilitates calcium absorption in the gut and helps regulate bone remodeling hormones. The NZ Ministry of Health recommends 1000mg of calcium daily for adults and up to 1500mg for those over 70. Vitamin D needs rise to 800-1000IU daily for seniors, especially in regions with limited sunshine.
Food sources are plentiful: dairy, leafy greens, fortified plant milks, and oily fish provide calcium, while sunlight, eggs, and fortified cereals boost vitamin D. When diet falls short, supplements can fill the gap, but it’s wise to check blood levels first to avoid excessive dosing.

Lifestyle Moves that Preserve Bone Mass
Exercise isn’t just about cardio; it’s a powerful bone‑building stimulus. Weight‑bearing activity includes any movement that forces you to support your own weight, such as walking, jogging, dancing, or resistance training triggers osteoblasts to lay down new bone. Studies from the University of Otago (2023) show that seniors who perform 150 minutes of weight‑bearing exercise per week retain up to 2% more bone density than inactive peers.
Balance training-tai chi, yoga, or simple heel‑to‑toe walks-reduces fall risk, a critical factor since most fractures in older adults result from a fall. Strengthening the core and lower‑leg muscles also improves stability when navigating uneven surfaces.
How to Detect Bone Damage Early
The gold‑standard screening tool is the DEXA scan (dual‑energy X‑ray absorptiometry) that measures bone mineral density (BMD) at the hip and spine. Results are expressed as a T‑score: a score of -1.0 or above is normal, between -1.0 and -2.5 signals osteopenia, and -2.5 or lower confirms osteoporosis.
General practitioners often recommend a DEXA test for women over 65 and men over 70, or earlier if you have risk factors such as a family history of fractures, long‑term corticosteroid use, or low body weight. The scan takes about 10 minutes, involves minimal radiation, and can be covered by public health schemes in New Zealand.
Treatment Options When Bone Loss is Detected
Medication isn’t the only answer, but for moderate to severe osteoporosis, pharmacologic therapy can cut fracture risk by up to 50%. Common classes include:
- Bisphosphonates (e.g., alendronate) - inhibit osteoclast activity.
- Selective estrogen receptor modulators (SERMs) - mimic estrogen’s protective effect on bone.
- Monoclonal antibodies like denosumab - target the RANKL pathway to reduce bone resorption.
- Hormone replacement therapy (HRT) - useful for post‑menopausal women with severe symptoms, but requires careful cardiovascular assessment.
All medications should be paired with calcium (1200mg) and vitamin D (800-1000IU) supplementation, plus a regular exercise routine.
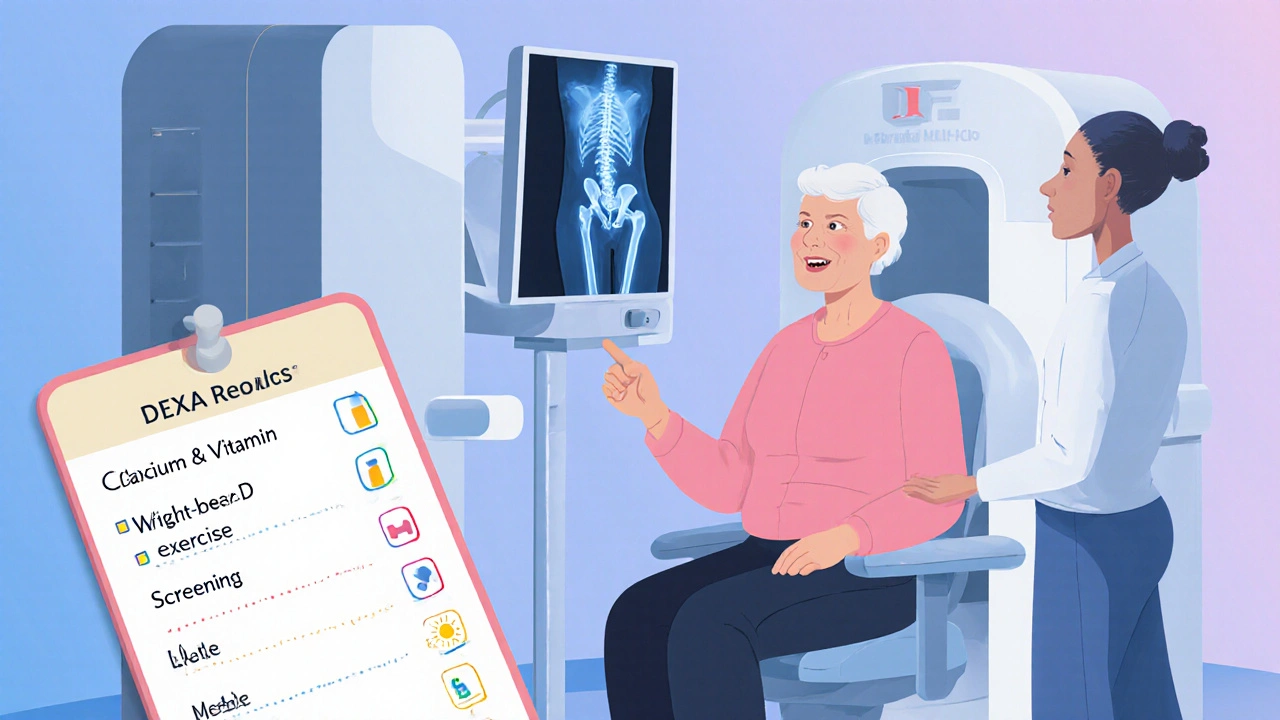
Practical Checklist for Maintaining Strong Bones
| Area | What to Do | Frequency / Target |
|---|---|---|
| Nutrition | Consume calcium‑rich foods and vitamin D sources | Daily: 1000‑1500mg Ca, 800‑1000IU D |
| Exercise | Weight‑bearing + resistance + balance training | 150min/week weight‑bearing, 2‑3sessions strength |
| Screening | Get a DEXA scan | Women≥65, Men≥70, or earlier with risk |
| Lifestyle | Avoid smoking, limit alcohol, maintain healthy weight | Ongoing |
| Medication (if prescribed) | Take as directed, monitor side‑effects | According to doctor’s schedule |
When to Seek Professional Help
If you notice any of the following, schedule a visit promptly:
- Sudden back pain or loss of height - could indicate a spinal fracture.
- Recurring joint pain not relieved by rest.
- Difficulty standing up from a chair or climbing stairs.
- Any fall that results in bruising, swelling, or inability to bear weight.
Early intervention can halt further bone loss and start the healing process.
Frequently Asked Questions
How often should I get a DEXA scan?
For most adults, a scan every 2-3 years is enough. If you’re on medication that affects bone density, your doctor may recommend annual testing.
Can men develop osteoporosis?
Yes. While less common than in women, men over 70 experience bone loss, especially if they have low testosterone, chronic steroid use, or a family history of fractures.
Is calcium supplement enough to prevent fractures?
Calcium alone helps maintain mineral content but doesn’t replace the mechanical stimulus that exercise provides. The best strategy mixes adequate calcium, vitamin D, and regular weight‑bearing activity.
What are the side effects of bisphosphonates?
Common issues include upset stomach, heartburn, or rare jaw osteonecrosis. Taking the pill with a full glass of water and staying upright for 30 minutes can reduce irritation.
Can I improve bone density after 70?
Absolutely. Studies show that consistent resistance training and proper nutrition can increase BMD by 1‑2% even in octogenarians, lowering fracture risk.
Drew Chislett
October 6, 2025 AT 14:36Nice rundown on bone health, especially the part about weight‑bearing exercise. It’s easy to forget that even a brisk walk can make a difference. The calcium‑vitamin D combo is classic, but I’d add magnesium for completeness. Keep it up, this info is genuinely useful.
Vanessa Guimarães
October 7, 2025 AT 10:02Oh sure, because everyone just loves another generic bone‑health checklist.
Lee Llewellyn
October 8, 2025 AT 05:29Look, I get that bone density matters, but the article glosses over the fact that most of these “recommendations” are just marketing fluff. You’re told to pop calcium pills, but the bioavailability is questionable without proper vitamin K2. And sure, DEXA scans sound high‑tech, yet they’re riddled with inter‑machine variability. The real problem is lifestyle-people binge‑watch Netflix while forgetting to stand up. Also, the hormonal angle is oversimplified; estrogen isn’t the only player. Men’s testosterone declines gradually, and diet plays a huge role. In short, the piece is good for a quick read, but it’s not a deep dive.
Rosalee Lance
October 9, 2025 AT 00:56When we consider the anatomy of aging, it’s almost poetic how the body reshapes itself. Bones, once resilient, become a subtle reminder of time’s passage. Yet, our choices-like embracing movement-can rewrite that narrative. The article nails the balance between nutrition and activity, which feels like a modern mantra. Keep pondering, because thought and action are two sides of the same bone.
Kara Lippa
October 9, 2025 AT 20:22Your checklist is clear and to the point. It’s a handy reference for anyone getting started.
Puneet Kumar
October 10, 2025 AT 15:49From an inclusive health perspective, integrating calcium‑rich legumes alongside dairy can bridge dietary gaps. Osteopenia, often an early flag, benefits from early lifestyle tweaks. The article’s emphasis on resistance training aligns with musculoskeletal physiology. Remember to personalize intensity based on baseline functional capacity.
michael maynard
October 11, 2025 AT 11:16Honestly, this feels like a lecture you’d get from a textbook. If you’re not already scared of your own bones, maybe try a real‑world scenario. I’d love to see some personal anecdotes instead of sterile bullet points.
Roger Bernat Escolà
October 12, 2025 AT 06:42Nice summary.
Allison Metzner
October 13, 2025 AT 02:09Did you know the government’s health agencies are funded by the supplement industry? It’s no coincidence they push calcium pills. The real cure is staying active, not swallowing pills. Question everything, especially the “official” advice.
william smith
October 13, 2025 AT 21:36Get a DEXA scan every 2‑3 years if you’re over 65.
Timothy Javins
October 14, 2025 AT 17:02While the article covers the basics, it neglects the socioeconomic barriers many face. Access to DEXA scans isn’t universal, and supplements can be pricey. Moreover, the piece assumes a one‑size‑fits‑all diet, ignoring cultural food variations. People in low‑income areas often rely on fortified cereals, not leafy greens. The narrative could be more inclusive of these realities. Still, the core message about movement is solid.
Kay Yang
October 15, 2025 AT 12:29I appreciate the balanced tone here – it’s neither preachy nor dismissive. The practical tips feel doable for most readers. It’s good to see both nutrition and exercise highlighted together. Thanks for sharing this concise guide.
Rajesh Kumar Batham
October 16, 2025 AT 07:56Great guide! 👍 The Vitamin D suggestions are especially helpful during winter. 🌞 Keep the info coming!
Bill Gallagher
October 17, 2025 AT 03:22First, let’s address the common misconception that calcium alone is a panacea; the literature shows synergistic effects with vitamin K2, magnesium, and phosphorus, each contributing to hydroxyapatite crystal formation in varying degrees of significance. Second, the article’s recommendation of “150 minutes per week” of weight‑bearing activity is a baseline, yet it fails to differentiate between low‑impact aerobics and high‑impact resistance training, which have distinct osteogenic potentials according to mechanotransduction studies. Third, the DEXA scan, while considered the gold standard, has limitations such as artefact susceptibility from spinal degenerative changes, leading to potential overestimation of bone density in older adults. Fourth, the piece mentions bisphosphonates but does not discuss the rare but serious adverse event of atypical femoral fractures, a crucial risk factor that influences prescribing decisions. Fifth, hormone replacement therapy is cited without emphasizing the need for individualized risk‑benefit analysis, especially concerning thromboembolic events. Sixth, the suggested calcium intake of 1000‑1500 mg per day overlooks dietary calcium’s variable absorption rates, which can be affected by oxalates and phytates present in certain plant foods. Seventh, the recommendation to limit alcohol is vague; research quantifies safe consumption as no more than two standard drinks per day for men and one for women, beyond which osteoclastic activity appears to increase. Eighth, smoking cessation is highlighted, yet the article does not elaborate on nicotine’s direct impact on osteoblast apoptosis, a nuanced mechanism detailed in recent endocrinology reviews. Ninth, the inclusion of “balance exercises” is valuable, but the article could benefit from specifying proprioceptive training protocols that have been shown to improve postural sway metrics. Tenth, regarding nutrition, the emphasis on dairy ignores lactose‑intolerant populations, for whom fortified plant milks provide comparable calcium bioavailability when fortified appropriately. Eleventh, the article’s table format is user‑friendly, yet it lacks a column for “frequency of monitoring,” which is critical for tracking progression in patients with osteopenia. Twelfth, while the text mentions “regular weight‑bearing activity,” it does not define frequency thresholds that differentiate between maintenance and therapeutic regimens. Thirteenth, the potential role of emerging therapeutics such as Romosozumab, a sclerostin‑inhibiting monoclonal antibody, is omitted despite its recent FDA approval for high‑risk patients. Fourteenth, the discussion of vitamin D supplementation does not address the debate over optimal serum 25‑hydroxyvitamin D levels, with some experts advocating for >30 ng/mL versus the traditional >20 ng/mL threshold. Finally, the article’s overall tone is supportive, but integrating these nuanced points would transform it from a general overview into a comprehensive, evidence‑based resource for clinicians and patients alike.
Rajashree Varma
October 17, 2025 AT 22:49That was an impressive deep‑dive, thank you for laying it all out. It’s reassuring to know there are layers of nuance beyond the headline advice. I’ll definitely keep those additional considerations in mind when discussing bone health with my patients.
Anshuman Pandey
October 18, 2025 AT 18:16Indeed, the interplay of micronutrients and mechanical loading reflects the body’s elegant adaptability. Let’s continue to bridge scientific detail with practical guidance.