Allergic rhinitis isn’t just a stuffy nose or a few sneezes. For millions, it’s a daily battle that disrupts sleep, drains energy, and makes outdoor life feel like a minefield. Whether it’s the pollen-heavy air of spring or the dust mites lurking in your bedding year-round, allergic rhinitis is more than an inconvenience-it’s a chronic condition that demands smart, consistent management. The good news? You don’t have to just live with it. With the right approach, most people can take back control of their breathing, their sleep, and their quality of life.
What’s Really Going On in Your Nose?
Allergic rhinitis happens when your immune system overreacts to harmless substances like pollen, dust mites, or pet dander. It’s not a cold. It’s not a virus. It’s an IgE-mediated inflammatory response-your body treats these allergens like invaders and launches a chemical attack. That’s what causes the runny nose, the itching, the sneezing fits, and the stubborn congestion. The trigger determines the pattern: seasonal allergic rhinitis flares up when specific plants pollinate, usually in spring, summer, or early fall. Perennial allergic rhinitis? That’s the year-round version, driven by indoor allergens that don’t take holidays.In New Zealand, tree pollen like birch and grasses like ryegrass are major offenders from October through December. Dust mites thrive in our humid coastal cities, especially in bedrooms where skin flakes accumulate. Mold spores rise after rain, and pet dander clings to carpets and furniture. Knowing your trigger is the first step-not just to avoid it, but to treat it properly.
First-Line Treatments: What Actually Works
There’s a lot of noise out there about allergy remedies. But clinical evidence points to two clear winners for most people: intranasal corticosteroids and second-generation oral antihistamines.Intranasal corticosteroids (like fluticasone, mometasone, or budesonide) are the gold standard for moderate-to-severe symptoms. They work by reducing inflammation deep in the nasal lining. Unlike decongestant sprays, they don’t cause rebound congestion. But they’re not fast. It takes 12 to 48 hours to feel the difference, and full effect can take up to two weeks. That’s why so many people give up too soon. If you’re using one and it doesn’t feel like a miracle on day three, don’t quit. Stick with it. Studies show consistent users get 30-50% better symptom control than those who don’t.
Oral antihistamines like cetirizine, loratadine, or fexofenadine are your go-to for quick relief of itching, sneezing, and runny nose. They start working in about an hour and don’t make you sleepy like the old-school ones (like diphenhydramine). But here’s the catch: they’re weak on congestion. If your nose is blocked, antihistamines alone won’t fix it. That’s why many people need both-a nasal spray for the blockage and an antihistamine for the itch.
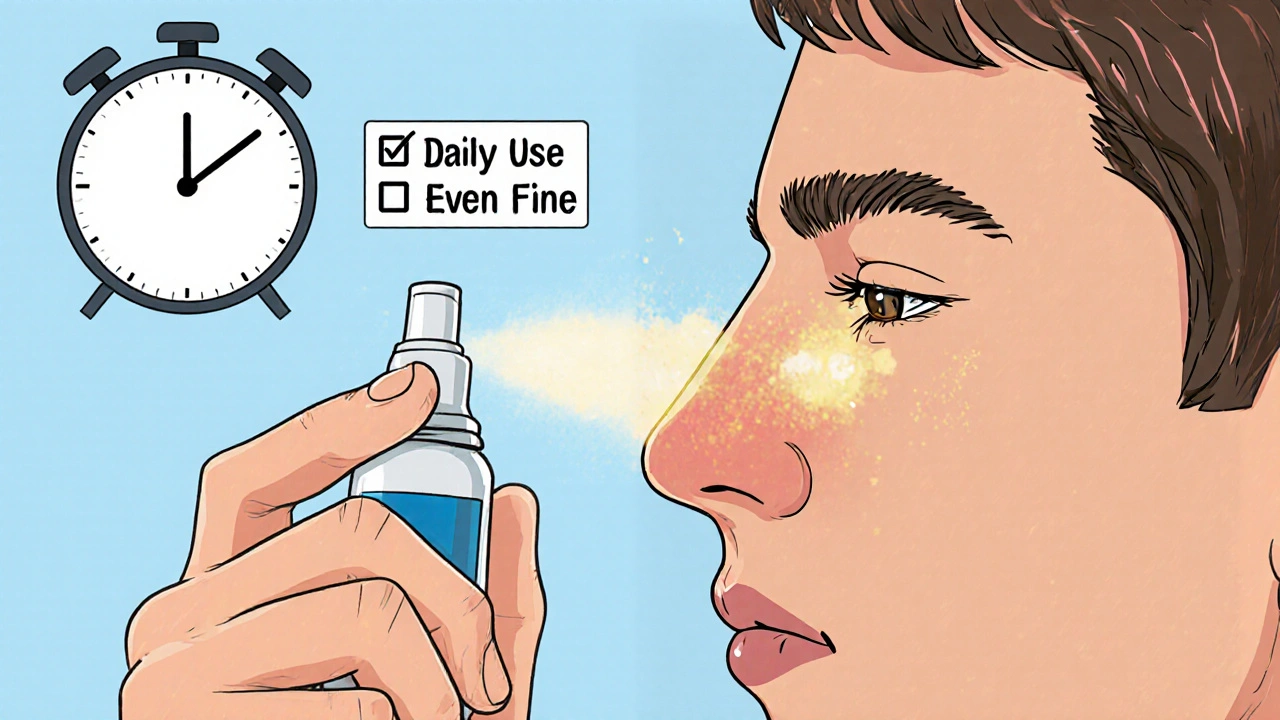
How to Use Your Nasal Spray Right (Most People Don’t)
Here’s a hard truth: up to 70% of people use their nasal corticosteroid spray incorrectly. And that cuts its effectiveness in half.Don’t aim it straight back toward your brain. That’s a common mistake. Instead, point the nozzle slightly outward-toward the outer wall of your nostril, not the middle. Gently inhale through your nose as you spray. Don’t snort hard. Then, avoid blowing your nose for at least 15 minutes after. This lets the medicine stick where it needs to.
And don’t use it only when you feel bad. These sprays work best when used daily, even on symptom-free days. Think of them like brushing your teeth-not a fix, but maintenance. Skipping doses because you’re feeling okay is like skipping flossing because your breath feels fine. It undermines the whole purpose.
When to Consider Immunotherapy
If you’ve tried the basics and still feel miserable, it’s time to think bigger. Immunotherapy-either shots or tablets-doesn’t just mask symptoms. It trains your immune system to stop overreacting.Sublingual immunotherapy (SLIT) tablets, like Grastek or Oralair, are now a mainstream option. You take them daily under your tongue, starting about four months before pollen season. They’re less scary than shots-you can take them at home after the first dose is monitored by a doctor. But they’re not magic. About 65% of users report mild oral itching at first. And 32% quit within the first year because it feels like a chore.
Subcutaneous immunotherapy (SCIT), or allergy shots, are slightly more effective, with 35-45% symptom reduction over time. But they require regular clinic visits for 3-5 years. The risk of a serious reaction is low-about 0.2% per shot-but it’s real. That’s why clinics keep epinephrine on hand.
Both options work best for people with clear, unavoidable triggers-like pollen or dust mites-and when medications aren’t cutting it. The American College of Allergy, Asthma & Immunology recommends considering immunotherapy if symptoms are severe, medications aren’t enough, or you want to reduce long-term drug use.
Environmental Control: The Quiet Hero
You can’t avoid all allergens. But you can reduce exposure dramatically with simple, practical steps.For dust mites: Wash bedding weekly in water hotter than 130°F (54°C). Use allergen-proof covers on your mattress and pillows. These aren’t fancy-just tightly woven fabric that blocks mites. Studies show they cut exposure by 83%. Keep indoor humidity below 50% with a dehumidifier. Mites drown in dry air.
For pollen: Check daily pollen counts (apps like Pollen Sense are accurate and free). Keep windows shut when counts are above 9.7 grains per cubic meter. Wear wraparound sunglasses outside-they reduce eye symptoms by 35%. Shower and change clothes after being outdoors. Pollen sticks to hair and fabric.
For pets: Keep them out of the bedroom. Wash your hands after petting them. Use a HEPA air purifier in high-use rooms. Vacuum weekly with a HEPA-filter vacuum.
For mold: Fix leaks. Clean bathroom mold with vinegar or bleach. Don’t let damp towels sit. Use exhaust fans after showers.
These aren’t radical changes. They’re habits. And they work. Many patients report fewer symptoms just from cleaning their bedroom and closing windows at night.
What Doesn’t Work (And Why)
Not everything you hear about allergies is true.Nasal decongestant sprays (like oxymetazoline) give fast relief-but only for three days max. After that, you get rebound congestion. Your nose becomes dependent. It’s a trap.
Oral decongestants (pseudoephedrine) help with stuffiness but raise blood pressure and can cause insomnia. Don’t use them longer than a week. And avoid them if you have high blood pressure or heart issues.
Saline rinses (neti pots or squeeze bottles) are safe and helpful. Many users report improvement, especially when used twice daily. But they’re a supplement-not a replacement-for medication. Don’t expect them to replace your nasal spray.
Herbal remedies and essential oils have no proven benefit for allergic rhinitis. Some, like eucalyptus oil, can irritate nasal passages and make symptoms worse.
The New Frontier: Biologics and Combination Therapies
In 2023, the FDA approved tezepelumab, the first biologic drug for allergic rhinitis. It targets a protein called TSLP that kicks off the allergic cascade. Early trials showed a 42% reduction in symptoms compared to placebo. It’s still new, expensive, and given by injection-so it’s not for everyone. But it’s a sign of where things are headed.More accessible right now are combination nasal sprays like azelastine/fluticasone. These deliver an antihistamine and a corticosteroid in one spray. They work faster than corticosteroids alone (within 30 minutes) and are more effective than either drug by itself. If you’ve struggled with delayed relief from nasal sprays, this might be your best bet.
When to See a Specialist
Most people try OTC antihistamines first. That’s fine. But if you’re still struggling after six weeks of consistent treatment, it’s time to see an allergist. The average time people wait before seeking help is over three years. That’s too long. You don’t need to suffer that long.Specialists can do allergy testing-skin prick or blood tests-to pinpoint exactly what you’re reacting to. That helps you tailor avoidance and decide if immunotherapy is right for you. They can also check for related conditions like asthma or sinusitis, which often go hand-in-hand with allergic rhinitis.
And if you’re a parent with a child who has allergies? Don’t wait. Studies show that kids with allergic rhinitis who get immunotherapy early have a 67% lower chance of developing asthma later.
Realistic Expectations
There’s no cure for allergic rhinitis. But there’s excellent control. Most people who follow a tailored plan-medication, environment, and sometimes immunotherapy-can live nearly symptom-free.Don’t expect perfection. Some days will be worse. Pollen counts spike. Your cat sheds more. Humidity rises. That’s normal. But if you’re using your nasal spray daily, avoiding major triggers, and staying consistent, you’ll notice a dramatic difference over time.
The biggest barrier isn’t the medicine. It’s patience. It’s remembering to use your spray when you feel fine. It’s washing your sheets even when you’re tired. It’s closing the window when you want to let in the breeze. These small actions add up.

fiona collins
November 25, 2025 AT 09:52Just moved to Wellington last year-finally got my nasal spray routine down. Used to think it was just ‘bad allergies,’ but after the allergist test, turns out I’m allergic to ryegrass and dust mites. Daily fluticasone + washing sheets in hot water? Game changer. No more 3 a.m. sneezing fits.
Agastya Shukla
November 26, 2025 AT 18:05From an immunology perspective, the IgE-mediated Th2 response in perennial rhinitis is particularly interesting because it often coexists with epithelial barrier dysfunction. The TSLP pathway mentioned in the biologics section is a key alarmin-its inhibition via tezepelumab represents a paradigm shift from symptom suppression to upstream cytokine modulation. Still, cost and access remain significant barriers in LMICs.
Karen Willie
November 28, 2025 AT 08:29I know it sounds boring, but using the spray correctly made all the difference for me. I used to aim it straight back like everyone does-and it never worked. Then I watched a 2-minute YouTube video on proper technique. Suddenly, I wasn’t waking up with a clogged nose. It’s not magic, it’s just science you have to do right.
Rachel Villegas
November 30, 2025 AT 02:25My mom had allergic rhinitis for 40 years and never tried immunotherapy until she was 65. She’s been on SLIT for 18 months now. She still takes her spray, but the sneezing fits? Gone. She says it’s the first time in decades she’s felt like she can breathe without thinking about it. If you’re on meds and still miserable, don’t give up-talk to an allergist.
Shivam Goel
December 1, 2025 AT 15:30Let’s be real-most of these ‘evidence-based’ recommendations ignore the placebo effect. People think they’re better because they’re using a spray daily, but the actual physiological improvement? Questionable. And don’t get me started on HEPA filters-studies show marginal benefit unless you’re living in a sealed bubble. Also, why is no one talking about the microbiome? Gut health affects nasal immunity. But nope, we’re all just spraying and washing sheets like it’s 1998.
Patricia McElhinney
December 1, 2025 AT 22:15Incorrect usage of intranasal corticosteroids is not merely a ‘common mistake’-it’s a catastrophic failure of patient education. The fact that 70% of users are misapplying these medications indicates systemic negligence by primary care providers. Furthermore, the recommendation to use antihistamines alongside corticosteroids is pharmacologically unsound in many cases, as it promotes polypharmacy without addressing root causes. And why is there no mention of leukotriene receptor antagonists? Montelukast is underutilized and far more effective than saline rinses.
Josh Zubkoff
December 3, 2025 AT 14:42Okay but have you ever WOKEN UP at 3am because your nose felt like a cement block and your eyes were swelling shut and you realized you forgot to close the window during that one thunderstorm and now you’re basically a walking allergy bomb? And then you spend the next 48 hours Googling ‘can you die from allergic rhinitis’ because your brain has been fried by lack of sleep and Benadryl? And then you find this post and you’re like… wait, I’ve been doing it wrong this whole time? Like I’ve been aiming the spray into my brain for 12 years? I’m not even mad. I’m just… exhausted. Also, my cat is now banned from the bedroom. And I bought a $200 HEPA filter. And I’m crying because I didn’t know I could feel this good. Thank you.
Amy Hutchinson
December 4, 2025 AT 06:04My cousin’s kid got allergy shots and now he’s ‘cured’-I swear he’s like a different person. No more asthma inhalers, no more missing school. I’m so done with OTC stuff. My doctor says I’m a candidate. I’m doing it next month. If you’re still suffering, just go. It’s not scary. I was scared too.
Aki Jones
December 4, 2025 AT 10:10Who funded this article? Big Pharma? Because tezepelumab is $30,000 a year and they’re pushing it like it’s the holy grail. Meanwhile, the real solution-removing synthetic fragrances, cleaning products, and plastic dust from homes-isn’t profitable. The entire medical system is built on selling you more sprays, not fixing the environment. And they call this ‘evidence-based’? Wake up. The ‘allergy epidemic’ isn’t genetic-it’s chemical. And they don’t want you to know that.
Josh Zubkoff
December 6, 2025 AT 08:07Wow, I didn’t even think about how much I’ve been avoiding the breeze. I used to love opening windows in the morning. Now I check pollen counts like I’m tracking a hurricane. And I swear, closing the window at night and showering after walking the dog? I haven’t needed a tissue since April. I didn’t think tiny habits would do that much. But they did.