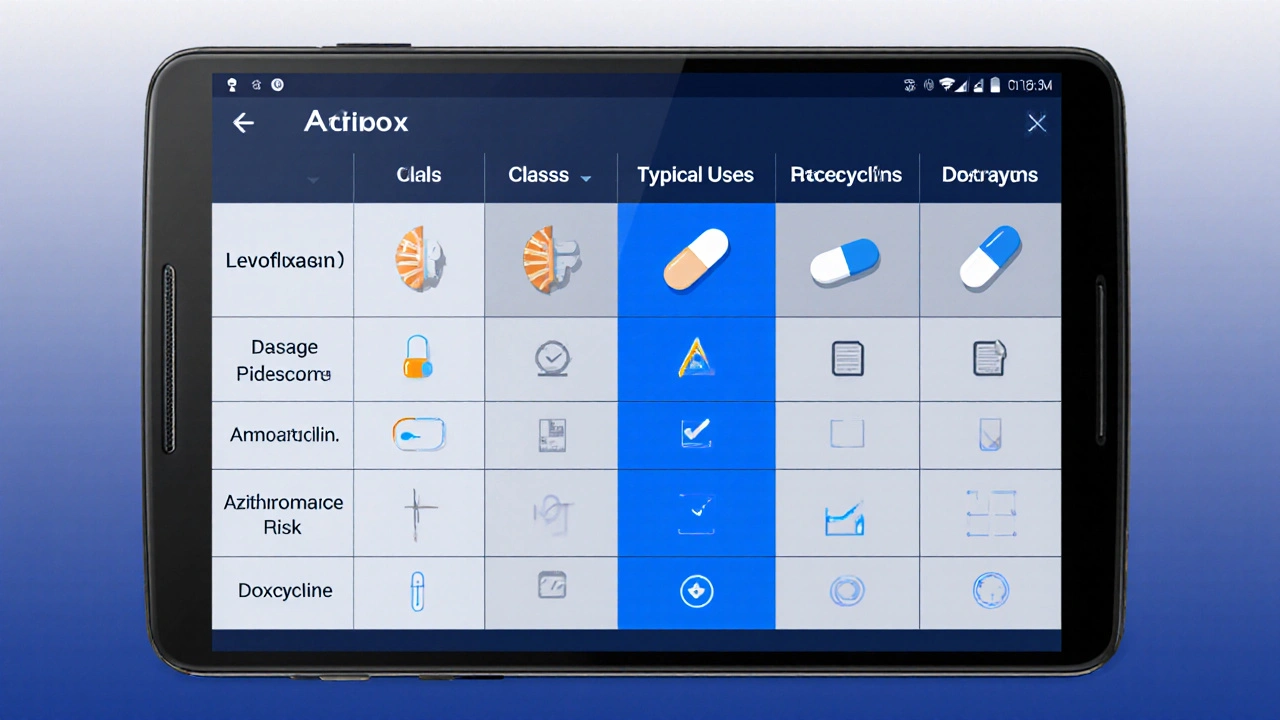
Ciplox vs Alternatives: Antibiotic Decision Helper
| Antibiotic | Class | Typical Use | Adult Dosage | Common Side Effects | Resistance Risk |
|---|
Select an infection type above to view personalized recommendations.
Understanding Ciplox and Its Place in Therapy
Ciplox belongs to the fluoroquinolones class. These drugs are prized for their ability to penetrate many tissue types and to kill gram‑negative organisms like Escherichia coli and Pseudomonas aeruginosa. Typical indications include uncomplicated urinary‑tract infections (UTIs), certain gastrointestinal infections (e.g., traveler's diarrhea), and skin infections where gram‑negative coverage is needed.
Standard adult dosing for Ciplox is 250‑750mg every 12hours, depending on infection severity. The drug is absorbed well from the gut, and most of the dose is eliminated unchanged via the kidneys - a fact that makes renal function a key dosing consideration.
How Ciplox Works - The Mechanism in Plain English
Imagine bacteria as a factory. To replicate, they need to copy their DNA. Ciplox throws a wrench into the factory’s copy machine - the DNA gyrase enzyme - causing the bacteria’s genetic material to become tangled and the cell to die. Because that enzyme is unique to bacteria, human cells are largely spared, which explains the drug’s good overall safety profile when used correctly.
Popular Alternatives - Quick Facts
Below is a side‑by‑side look at five widely used antibiotics that clinicians often consider instead of Ciplox. The table includes the drug’s class, typical infections treated, adult dosage, common side effects, and a note on resistance trends.
| Antibiotic | Class | Typical Use | Adult Dosage | Common Side Effects | Resistance Risk |
|---|---|---|---|---|---|
| Ciplox (Ciprofloxacin) | Fluoroquinolone | UTI, traveler's diarrhea, skin infections | 250‑750mg PO q12h | Tendonitis, QT prolongation, GI upset | Increasing, especially in E. coli |
| Levofloxacin | Fluoroquinolone | Community‑acquired pneumonia, sinusitis | 500‑750mg PO q24h | Headache, photosensitivity, tendon issues | Moderate, similar patterns to ciprofloxacin |
| Amoxicillin | Penicillin | Otitis media, streptococcal pharyngitis, dental infections | 500‑875mg PO q8h | Rash, diarrhea, rarely liver enzymes rise | Low for typical strains, high for β‑lactamase producers |
| Azithromycin | Macrolide | Chlamydia, atypical pneumonia, bronchitis | 500mg PO day1, then 250mg qd days2‑5 | GI upset, QT prolongation (rare) | Rising in Mycoplasma and some gonorrhea strains |
| Doxycycline | Tetracycline | Rickettsial diseases, acne, Lyme disease | 100mg PO q12h | Photosensitivity, esophageal irritation | Generally low, but some S. aureus strains resistant |

When to Choose Ciplox Over the Alternatives
1. Gram‑negative dominance: If lab cultures indicate E.coli, Klebsiella, or Pseudomonas, a fluoroquinolone like Ciplox often clears the infection faster than penicillins or macrolides.
2. Kidney‑friendly dosing: Because Ciplox is eliminated renally, dosing can be tailored easily for patients with reduced kidney function, unlike drugs that rely on hepatic metabolism.
3. Shorter course: Many Ciplox regimens finish in 5-7days, whereas amoxicillin for sinusitis might run 10days. Shorter exposure can improve compliance.
4. Travel‑related diarrhea: In regions where resistance to azithromycin is climbing, ciprofloxacin remains a first‑line agent for Campylobacter‑type diarrhea, provided the local susceptibility data support it.
5. Cost considerations: Generic ciprofloxacin is often cheaper than newer macrolides or tetracyclines, making it a budget‑friendly choice for many health systems.
Safety Profile - What to Watch For
Fluoroquinolones have earned a reputation for rare but serious side effects. The FDA now warns about tendon rupture, especially in patients over 60, those on steroids, or athletes. If a patient feels sudden calf or shoulder pain, they should stop the drug and seek medical advice.
Other notable concerns include:
- QT interval prolongation - caution in patients with cardiac arrhythmias or on other QT‑prolonging meds.
- Peripheral neuropathy - symptoms like tingling or numbness can be irreversible.
- Clostridioides difficile infection - a risk shared with many broad‑spectrum antibiotics.
Most alternatives have milder safety warnings. For example, amoxicillin rarely causes severe allergic reactions, and azithromycin’s biggest risk is modest QT prolongation, but it’s often considered safer for pregnant women.
Practical Tips for Patients and Prescribers
- Confirm the pathogen: Whenever possible, get a urine culture or throat swab before starting Ciplox. Targeted therapy reduces resistance.
- Hydration matters: Drinking plenty of water helps flush the drug and reduces crystal formation in the kidneys.
- Take with food? Ciplox can be taken with or without meals, but avoid dairy or antacids within two hours as they bind the drug and lower absorption.
- Complete the course: Even if symptoms improve, finish the prescribed days to prevent lingering bacteria.
- Monitor for tendon pain: Advise patients to stop sport or heavy lifting until therapy ends.
Frequently Asked Questions
Is Ciplox safe for children?
Ciplox is generally avoided in children under 18 unless no safer alternative exists, because fluoroquinolones have been linked to joint cartilage damage in animal studies. Pediatric infections are usually treated with amoxicillin or macrolides.
Can I take Ciplox with my blood pressure medication?
Most antihypertensives are fine, but avoid combining Ciplox with drugs that affect heart rhythm (e.g., sotalol) because of additive QT‑prolongation risk. Always check with a pharmacist.
Why is my doctor switching me from Ciplox to Levofloxacin?
Levofloxacin offers once‑daily dosing, which many patients find easier. It also has slightly less tendon‑related risk, though both belong to the same class. The switch is usually a convenience choice.
What should I do if I develop a rash while on Ciplox?
Stop the medication and seek medical attention immediately. A rash could signal an allergic reaction, which may progress to Stevens‑Johnson syndrome in rare cases.
Is there a risk of antibiotic resistance with short courses?
Short, appropriate courses actually lower resistance pressure compared to prolonged, unnecessary use. The key is using the right drug for the right bug, which is why culture‑guided therapy is recommended.

Bottom Line
Choosing between Ciplox and its alternatives boils down to the infection type, bacterial susceptibility, patient health profile, and safety concerns. Ciplox shines against gram‑negative urinary and gut bugs, offers a cheap short‑course option, and is easy to dose for kidney‑adjusted patients. However, its tendon and cardiac warnings mean clinicians often reserve it for cases where other drugs-like amoxicillin for throat infections or azithromycin for atypical pneumonia-won’t do the job.
Talk to your prescriber about the specific pathogen, any existing heart or tendon issues, and whether a narrower‑spectrum drug could be just as effective. In the end, the right antibiotic is the one that clears the infection fast while keeping side effects to a minimum.
Karen Gizelle
October 3, 2025 AT 16:00We really need to think about the moral weight of handing out Ciplox like candy. Overprescription fuels resistance, and that's not just a medical issue-it’s an ethical one. Doctors should ask themselves if a narrower drug could do the job before reaching for a fluoroquinolone. It's imortant to protect future patients from a world where common infections become untreatable.
Stephanie Watkins
October 4, 2025 AT 19:46Thanks for the thorough breakdown.
Zachary Endres
October 5, 2025 AT 23:33Wow, this tool makes picking the right antibiotic feel like a superpower! If you follow the guidance, you’ll avoid a lot of headaches later. Keep up the good work, everyone!
Ashley Stauber
October 7, 2025 AT 03:20I just don’t buy the hype around fluoroquinolones. Most of the time a simple amoxicillin will do and you avoid the tendon drama. Let’s stop glorifying a drug that’s overused.
Raghav Narayan
October 9, 2025 AT 10:53From a clinical pharmacology perspective, ciprofloxacin’s pharmacokinetic profile warrants a nuanced discussion. The drug achieves high urinary concentrations, making it particularly efficacious in uncomplicated urinary tract infections where the pathogen load is predominantly gram‑negative. However, the rising prevalence of quinolone‑resistant Escherichia coli strains in community settings has eroded that advantage, as evidenced by surveillance data from multiple geographic regions. When resistance rates exceed 10‑15 percent, empiric therapy with ciprofloxacin becomes questionable, and clinicians should consider alternatives such as nitrofurantoin or fosfomycin, which retain activity against resistant isolates. Moreover, the drug’s elimination is primarily renal, allowing dose adjustment in patients with impaired kidney function, yet this same pathway predisposes to crystal formation and potential nephrotoxicity if adequate hydration is not maintained. The adverse‑effect profile, while generally tolerable, includes rare but serious events such as Achilles tendon rupture, especially in patients over sixty years of age, those on systemic corticosteroids, or individuals engaged in high‑impact exercise. Cardiac safety is another consideration; quinolones can prolong the QT interval, necessitating caution in patients with known arrhythmias or concomitant use of other QT‑prolonging agents. In addition, the drug’s impact on the gut microbiome can predispose to Clostridioides difficile infection, a complication that further emphasizes the need for judicious prescribing. From an antimicrobial stewardship standpoint, the principle of using the narrowest effective agent should guide therapy, reserving ciprofloxacin for situations where its spectrum offers a clear benefit, such as documented Pseudomonas infections or when oral therapy is required for organisms resistant to beta‑lactams. Finally, cost considerations, while often favorable for generic ciprofloxacin, must be weighed against the potential downstream costs of managing adverse events and resistant infections. In summary, ciprofloxacin remains a valuable tool in the armamentarium, but its use should be individualized, evidence‑based, and aligned with stewardship goals to preserve its efficacy for future patients.
Tara Phillips
October 10, 2025 AT 14:40Esteemed readers, I encourage you to reflect upon the data presented and to apply it with both rigor and compassion. Selecting an antibiotic is not merely a clinical decision but also a stewardship responsibility.
Derrick Blount
October 11, 2025 AT 18:26May I point out, for the sake of precision, that the term “fluoroquinolone” should be capitalized when used as a class name; moreover, the dosage range of 250‑750 mg is not merely a suggestion, it is a protocol, and the phrase “typical use” ought to be enclosed in quotation marks to denote its status as a defined field. Additionally, one might argue that the side‑effect list is incomplete without mentioning, for example, photosensitivity; consequently, the table would benefit from a footnote clarifying these omissions.
Anna Graf
October 12, 2025 AT 22:13Choosing an antibiotic is like picking a key; the right one opens the door to health.
Jarrod Benson
October 14, 2025 AT 02:00Hey folks, just wanted to drop a quick note that this interactive tool is seriously handy. It’s not every day you get a clean layout that shows you the pros and cons of each drug at a glance. If you’re ever stuck deciding between Ciplox and something like amoxicillin, just hit the dropdown and let the table do the heavy lifting. And remember, staying hydrated while on any antibiotic helps your kidneys clear the meds faster, so keep that water bottle handy. Keep learning and stay healthy, everyone!
Liz .
October 15, 2025 AT 05:46Cool info, love the table!
tom tatomi
October 16, 2025 AT 09:33Sounds intense 😐
Tom Haymes
October 17, 2025 AT 13:20Balancing efficacy with safety is the hallmark of good prescribing. Remember that the narrowest spectrum that will reliably clear the infection should be your first choice; it protects the microbiome and reduces resistance pressure.
Scott Kohler
October 18, 2025 AT 17:06Ah, yes, because the pharmaceutical industry surely has no interest in profit, and every physician is a saintly guardian of public health-how refreshing.
Brittany McGuigan
October 19, 2025 AT 20:53The data clearly indicate thes specific advantages of ciplox, especially in gram‑negative crases. However, one must not overlook the potential risks associated wih long‑term use.
Priya Vadivel
October 21, 2025 AT 00:40Thank you for the thorough explanation; I appreciate how you highlighted both the benefits and the cautions. It really helps clinicians make more informed choices, especially when considering patient‑specific factors.
Dharmraj Kevat
October 22, 2025 AT 04:26Drama unfolds-antibiotics clash, choices made, lives saved.
Lindy Fujimoto
October 23, 2025 AT 08:13Wow, such a thorough guide! 😍👏 It’s like having a mini‑pharmacy in your browser.