For decades, people have been told that generic drugs are just as good as brand-name ones-but still, many hesitate. Maybe you’ve heard stories about someone who switched to a generic and felt worse. Or maybe you’re worried the cheaper version isn’t really the same. You’re not alone. But here’s the truth: generic drugs are not a compromise. They’re a scientifically proven alternative that works just as well for most people-and saves you a lot of money.
What Exactly Is a Generic Drug?
A generic drug is the exact same medicine as its brand-name counterpart, just sold under a different name. It contains the same active ingredient, in the same strength, same form (pill, injection, cream, etc.), and works the same way in your body. The FDA requires it to meet the same strict standards for quality, purity, and potency. The only differences? The color, shape, flavor, or filler ingredients-things that don’t affect how the medicine works. For example, the generic version of Lipitor is atorvastatin. The generic version of Nexium is esomeprazole. The active ingredient is identical. The FDA doesn’t allow a generic to be sold unless it’s proven to do the same job as the brand.How Do We Know Generics Work the Same?
Before a generic drug hits the shelf, it must pass a test called bioequivalence. This means researchers give the generic and the brand-name drug to healthy volunteers and measure how much of the drug enters the bloodstream and how fast. The results must fall within 80% to 125% of the brand’s performance. That’s not a wide range-it’s tight enough to ensure the body reacts almost identically. This isn’t a guess. It’s a legal requirement. The FDA reviews data from studies involving 24 to 36 people, using precise lab equipment and controlled conditions. Over 99.8% of approved generics meet or exceed this standard. And the manufacturing facilities? They’re held to the same rules as brand-name makers. In 2022, 98.7% of generic drug plants passed FDA inspections-slightly higher than brand-name plants.Myth: Generics Are Made in Poor-Quality Factories
A lot of people think generics come from sketchy overseas labs. But that’s not true. The FDA inspects every facility that makes drugs sold in the U.S.-whether it’s in Indiana or India. In fact, many brand-name drugs are made in the same factories as generics. The difference? The brand pays for marketing. The generic doesn’t. The FDA’s 2023 Drug Shortage Report found that 78% of active ingredients come from China and India. That’s not because those countries are less safe-it’s because they produce them more efficiently. And yes, the FDA sends inspectors there regularly. If a plant fails, it’s shut down. No exceptions.Myth: Generics Cause More Side Effects
There are stories online about people having bad reactions after switching to generics. But most of the time, it’s not the active ingredient causing the problem-it’s the inactive stuff. Inactive ingredients are things like dyes, fillers, or preservatives. They don’t treat your condition, but they can trigger allergies. For example, someone allergic to red dye might react to a red generic pill but not a white brand-name one. Or a person with lactose intolerance might feel bloated if the generic uses lactose as a filler and the brand doesn’t. That’s why it’s important to check the label. The FDA says 67% of generic drug labels don’t list all inactive ingredients clearly-compared to 99% for brand-name drugs. If you notice a new reaction after switching, talk to your pharmacist. They can check the ingredients and help you find a version without the trigger.
Myth: Generics Are Less Effective for Serious Conditions
Some conditions need extra care. Drugs with a narrow therapeutic index (NTID) are tricky. That means the difference between a dose that works and one that’s dangerous is very small. Examples include warfarin (blood thinner), levothyroxine (thyroid), and phenytoin (seizure control). For these, the FDA requires tighter bioequivalence standards: 90% to 112% instead of 80% to 125%. And many doctors prefer to keep patients on the same manufacturer’s version once they’ve found one that works. That’s not because generics are inferior-it’s because even tiny differences in how the drug dissolves can matter in these cases. But here’s the key: most NTID generics still work perfectly. A 2020 study in Nature looked at 17 cardiovascular drugs and found that patients on generics had fewer heart attacks and deaths than those on brand names. Another study in 2019 showed generic amlodipine lowered cardiovascular risk more than the brand. For most people, generics are just as safe-or safer.What About the Bad Stories?
Yes, there are rare cases where a patient had trouble after switching. One Reddit user reported erratic thyroid levels after switching from Synthroid to generic levothyroxine. Another case involved seizures returning after switching from Keppra to generic levetiracetam. These are real. But they’re also rare. A 2024 study of 2,450 patients found 74.9% had no issues at all. Consumer Reports surveyed 1,200 users and found 82% said generics worked exactly like the brand. Only 7% noticed any difference. The problem? When a patient has a bad experience, they’re more likely to tell someone than when everything goes fine. That creates a skewed perception. It’s like thinking all planes are unsafe because you heard about one crash.Why Do Some Doctors Hesitate?
Some doctors still prefer brands-not because they doubt generics, but because they’ve seen patients struggle after a switch. They worry about confusion, adherence, or rare reactions. A 2021 study found that adherence dropped by 5.3% in the first 90 days after switching to a generic. Why? Because patients thought the new pill was “weaker” or “fake.” That’s a perception issue, not a drug issue. Education helps. When patients understand why generics are cheaper and just as effective, they stick with them. Doctors who work in hospitals know this. Ninety-eight percent of U.S. hospitals use generics as their first choice. Why? Because they save millions without sacrificing care.
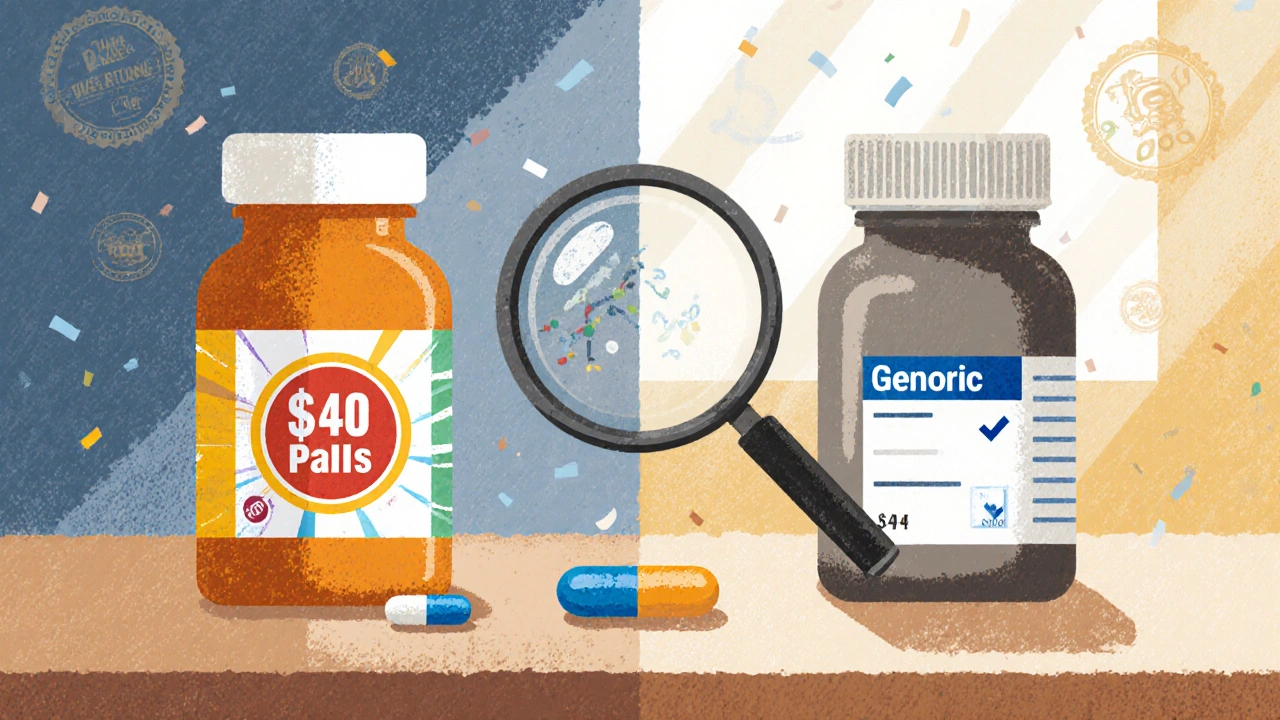
How Much Money Do Generics Save?
Between 2010 and 2020, generic drugs saved the U.S. healthcare system $2.29 trillion. That’s more than the GDP of most countries. In 2022, generics made up 90.2% of all prescriptions filled-but only 19.3% of total drug spending. A brand-name drug might cost $300 a month. The generic? $20. That’s not a small difference. It’s the difference between taking your medicine and skipping it because you can’t afford it. And globally, the generic drug market is growing fast. It’s expected to hit $725 billion by 2028. That growth isn’t happening because people are desperate. It’s happening because it works.When Should You Be Careful?
Most of the time, generics are safe. But here’s when to pay extra attention:- Narrow therapeutic index drugs: Levothyroxine, warfarin, phenytoin, digoxin. Stick with the same manufacturer if possible.
- Complex formulations: Inhalers, creams, patches. These are harder to copy exactly. The FDA is working on new standards for these.
- Psychiatric meds: Some studies show slightly higher hospitalization rates with generic escitalopram or sertraline. Not always-but worth monitoring.
- Allergies: Always check the inactive ingredients if you’ve had reactions before.
What Can You Do?
You don’t need to fear generics. But you do need to be informed.- Ask your pharmacist: “Is this generic? What’s the manufacturer?”
- Check the label for inactive ingredients if you have allergies.
- Don’t switch brands randomly. If you’re stable on a generic, stay on it.
- If you feel different after switching, don’t assume it’s the drug. Talk to your doctor. Track your symptoms. Get blood tests if needed.
- Use the FDA’s Orange Book to look up which generics are approved for your drug.
The Bottom Line
Generic drugs are not second-rate. They’re the result of decades of science, strict regulation, and billions of doses taken safely. For most people, they’re just as safe and effective as brand-name drugs-and far more affordable. The rare cases where problems occur aren’t proof that generics don’t work. They’re reminders that medicine isn’t one-size-fits-all. But those exceptions don’t cancel out the overwhelming evidence: generics save lives, reduce costs, and deliver the same results. If you’re worried, talk to your doctor or pharmacist. Don’t let myths stop you from taking what you need.Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet identical standards for quality, purity, and potency. Manufacturing facilities for generics are held to the same strict rules as brand-name makers, and over 99.8% of approved generics meet bioequivalence standards.
Why are generic drugs so much cheaper?
Generic drugs cost less because they don’t need to repeat expensive clinical trials. The brand-name company already proved the drug is safe and effective. Generic manufacturers only need to show their version is bioequivalent-saving millions in development costs. They also don’t spend money on advertising or fancy packaging.
Can switching to a generic cause side effects?
Rarely, and usually not because of the active ingredient. Side effects after switching are often due to differences in inactive ingredients like dyes, fillers, or preservatives. People with allergies or sensitivities may react to these. If you notice new symptoms after switching, check the label or ask your pharmacist for a different generic version.
Are generics okay for thyroid medication like levothyroxine?
Yes, most people do fine on generic levothyroxine. But because it’s a narrow therapeutic index drug, even small changes in absorption can affect thyroid levels. The FDA requires tighter bioequivalence standards for these drugs. If you’re stable on a brand or a specific generic, it’s often best to stay on it. If you switch, get your TSH levels checked after 6-8 weeks.
Do hospitals use generic drugs?
Yes. 98% of U.S. hospitals use generics as their first-line treatment for most conditions. They do this because generics are proven to work just as well and save millions of dollars without compromising patient outcomes. Many health systems automatically substitute generics unless the doctor specifically requests the brand.
How do I know if a generic is right for me?
Talk to your doctor or pharmacist. Ask if your medication has a narrow therapeutic index, if you have allergies to fillers, or if you’ve had issues with previous switches. For most people, generics are safe and effective. If you’re unsure, start with a small refill and monitor how you feel. Track any changes and report them.
Miriam Lohrum
November 27, 2025 AT 04:09It’s funny how we trust a pill more when it has a fancy name and a $300 price tag. The science doesn’t care about branding. It just cares about molecules. If the active ingredient is identical, the body doesn’t know the difference. We’re not saving money-we’re just getting over our own ego.
Generics aren’t ‘cheap.’ They’re efficient. And efficiency shouldn’t be a dirty word in medicine.
archana das
November 28, 2025 AT 15:43In India, we grow up with generics. My grandma takes her blood pressure pills from a local pharmacy-no name, just a little green tablet. She’s 82, walks every morning, and never missed a dose. Why? Because it works. Brand names are for ads, not for life.
People fear what they don’t understand. But medicine isn’t about logos. It’s about healing.
Jonah Thunderbolt
November 30, 2025 AT 04:39Okay, but let’s be real-this whole ‘generics are fine’ narrative is just Big Pharma’s way of gaslighting the middle class into accepting subpar care. I’ve seen people on generics crash. I’ve seen labs go wild. And no, it’s not ‘inactive ingredients.’ It’s the fact that the FDA lets these things through with half the scrutiny.
Also, if you think 99.8% is good enough… you’re not thinking hard enough. 🤡💊
Gayle Jenkins
December 1, 2025 AT 03:01STOP letting fear control your health decisions. If you’re worried about your thyroid med, get your TSH checked after switching-not because generics are bad, but because your body deserves monitoring. That’s not fear-that’s responsibility.
And if you think paying $300/month for a pill is ‘worth it’ because it’s got a logo on it, you’re not saving money-you’re being scammed. Talk to your pharmacist. Ask questions. Be proactive. Your life is worth more than a placebo brand.
Also, if you’re on warfarin and you switch manufacturers, yes-check your INR. But that’s true for BRANDS too. Consistency matters. Not the label.
Kaleigh Scroger
December 1, 2025 AT 04:54Most people don’t realize that the FDA doesn’t even test every batch of generic drugs. They test the manufacturing process and the bioequivalence study and assume consistency. That’s fine for most drugs but for NTIDs like levothyroxine or phenytoin that’s a gamble. You can have two generics from the same company with different dissolution rates because the fillers changed slightly. And yeah that’s legal. And yeah that’s dangerous for some.
It’s not that generics are bad. It’s that we treat them like they’re interchangeable when they’re not. The system assumes uniformity but biology doesn’t care about assumptions. If you’re on a narrow window drug and you switch? Track your numbers. Don’t just trust the label. And if your doctor doesn’t know this? Find a new one.
Also the claim that 98.7% of generic plants pass inspections is misleading because they inspect for paperwork more than actual product quality. The FDA is understaffed and overwhelmed. Don’t mistake compliance for safety.
And don’t get me started on how many generics are made in the same factory as the brand but labeled differently. That’s not transparency. That’s corporate obfuscation.
Bottom line: generics are not inherently unsafe. But the system that regulates them is not designed to protect you. It’s designed to keep costs low. There’s a difference.
Elizabeth Choi
December 1, 2025 AT 23:27Let’s not pretend this is about science. It’s about profit. The fact that 78% of active ingredients come from China and India means we’re outsourcing our health to countries with no real accountability. The FDA can’t inspect every factory. They send inspectors once every 5 years. Meanwhile, the FDA’s own reports show 20% of generic drug facilities have serious violations. And you’re telling me that’s okay?
Also, the ‘99.8% meet standards’ stat is meaningless if you’re in the 0.2%. You don’t get to be a statistic when your seizure comes back.
Generics aren’t evil. The system is.
Cecily Bogsprocket
December 3, 2025 AT 17:09I used to be terrified of generics after my cousin had a bad reaction to one. But I sat down with my pharmacist and we looked at the ingredients together. Turns out, it was the red dye. Same pill, different color. I switched to a white version and never looked back.
It’s not about the drug. It’s about the details. And most people don’t know how to ask the right questions.
My dad’s on generic warfarin and he’s fine. He gets his INR checked every 6 weeks. That’s the real key-not avoiding generics, but staying engaged. Medicine isn’t passive. It’s a conversation.
And honestly? I’m grateful for generics. My mom couldn’t afford her heart meds before. Now she takes them every day. That’s not a compromise. That’s justice.
Leo Adi
December 5, 2025 AT 01:03Back home in Kerala, we call them ‘copy pills.’ Everyone knows what they are. No one cares. If it works, it’s good. If it doesn’t, you go back. Simple.
Here in the US, it’s all about branding. Like buying a phone just because it has an apple on it. Medicine isn’t a status symbol. It’s a tool.
Melania Rubio Moreno
December 5, 2025 AT 14:32generic drugs arent even real drugs lol they just put chalk and hope in a capsule and call it a day. my uncle took one and started hallucinating. it wasnt the active ingrediant it was the… uh… the magic dust? idk but it wasnt right.
Gaurav Sharma
December 6, 2025 AT 06:36It is a matter of grave concern that regulatory frameworks in developed nations have become so permissive that substandard pharmaceutical products are permitted under the guise of cost-efficiency. The bioequivalence thresholds are scientifically indefensible. This is not healthcare. It is commodification.
Shubham Semwal
December 7, 2025 AT 20:07you people act like generics are magic. they’re not. if your thyroid meds stop working after switching, you’re not crazy-you’re just unlucky. and yeah, you should’ve stayed on the brand. but now you’re stuck paying 15x more just because you didn’t do your homework. welcome to capitalism.
Sam HardcastleJIV
December 9, 2025 AT 06:10One might reasonably posit that the proliferation of generic pharmaceuticals, while economically expedient, constitutes a latent erosion of the therapeutic contract between physician and patient. The absence of brand fidelity introduces a variable of uncertainty that, in the context of chronic disease management, is neither negligible nor ethically benign.
Mira Adam
December 11, 2025 AT 01:52Of course generics work. That’s not the point. The point is that we’ve been conditioned to accept lower standards because we’re too lazy to demand better. And now we’re surprised when people get sick? Shocking.