If you’ve ever woken up with a burning chest or a sour taste in your mouth, you’re not alone. About 7% of adults deal with daily acid reflux, and for many, it’s not just an occasional annoyance-it’s chronic GERD. The good news? You don’t have to live with it. The better news? The most effective way to manage GERD isn’t just popping pills-it’s combining smart lifestyle changes with the right medication, when needed.
What Actually Happens in GERD?
GERD isn’t just heartburn. It’s a condition where the lower esophageal sphincter (LES), the muscle that acts like a door between your stomach and esophagus, doesn’t close tightly. That lets stomach acid-strong enough to dissolve metal-flow back up into your esophagus. Your stomach lining can handle it. Your esophagus can’t. That’s when you feel the burn, the sour taste, or even a chronic cough. The American College of Gastroenterology defines GERD as symptoms happening at least twice a week. And it’s not just about discomfort. Left untreated, GERD can lead to Barrett’s esophagus, a precancerous change in the esophagus lining that affects 10-15% of long-term sufferers. It can also cause strictures-narrowing of the esophagus-that make swallowing painful or impossible.PPIs: The Heavy Hitters of Acid Control
Proton pump inhibitors (PPIs) like omeprazole, pantoprazole, and esomeprazole are the most powerful acid-reducing drugs available. They work by shutting down the acid-producing pumps in your stomach cells. Unlike antacids that just neutralize acid already there, or H2 blockers that reduce acid by about 60-70%, PPIs cut production by 90-98%. In clinical trials, PPIs heal esophagitis (inflammation from acid damage) in 70-90% of cases. That’s why they’re the first-line medication for moderate to severe GERD or when damage is visible on an endoscopy. But here’s the catch: PPIs aren’t magic. They take 1-4 hours to start working and need to be taken 30-60 minutes before your first meal of the day. Taking them after breakfast? You’re wasting them.The Hidden Costs of Long-Term PPI Use
PPIs are effective-but they’re not harmless. Studies show that using them for more than a year increases your risk of:- Enteric infections like C. diff (20-50% higher risk)
- Vitamin B12 deficiency (due to reduced acid needed for absorption)
- Acute interstitial nephritis (a type of kidney inflammation)
- Higher hip fracture risk in older adults (35% increase with 3+ years of use)
Lifestyle Changes: The Foundation No Pill Can Replace
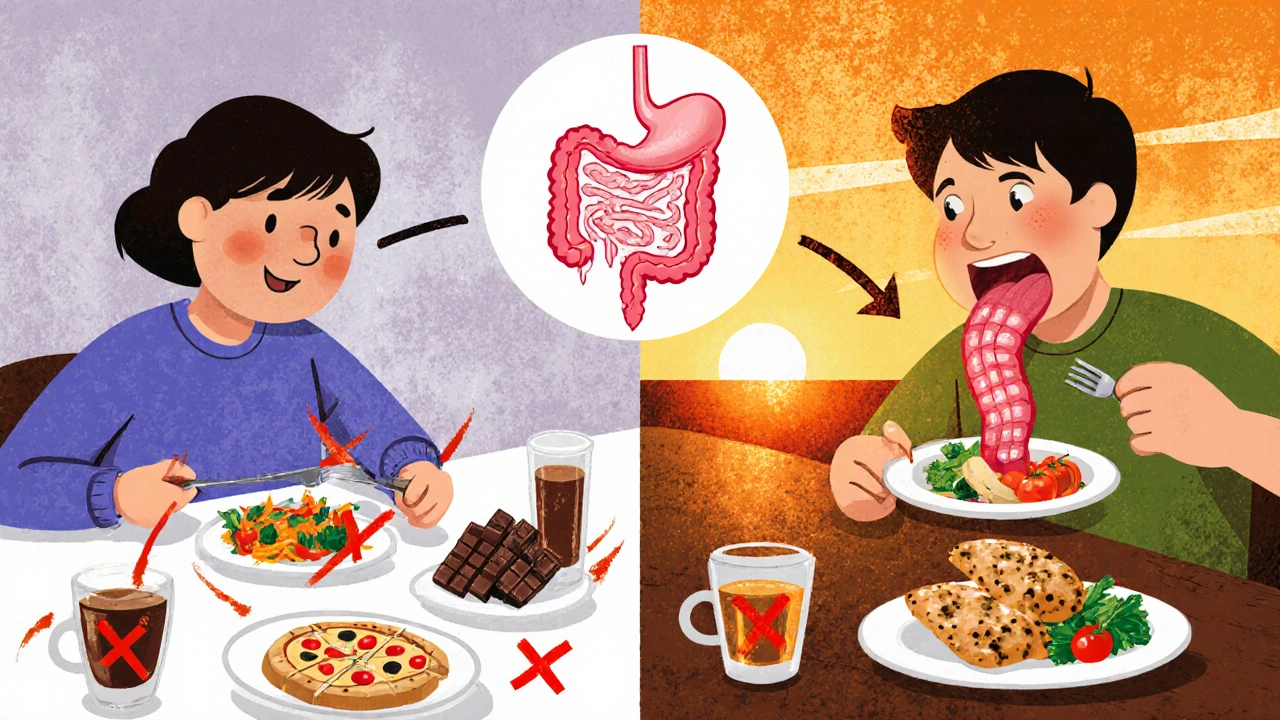
Medication helps, but lifestyle changes are the only treatment that addresses the root cause. And the data is clear:- Losing just 5-10% of your body weight reduces GERD symptoms by 50%.
- Avoiding food within 2-3 hours of bedtime cuts nighttime acid exposure by 40-60%.
- Eliminating trigger foods like coffee, tomatoes, alcohol, chocolate, and fatty or spicy foods helps 70-80% of people.
What Works Best? The Stepwise Approach
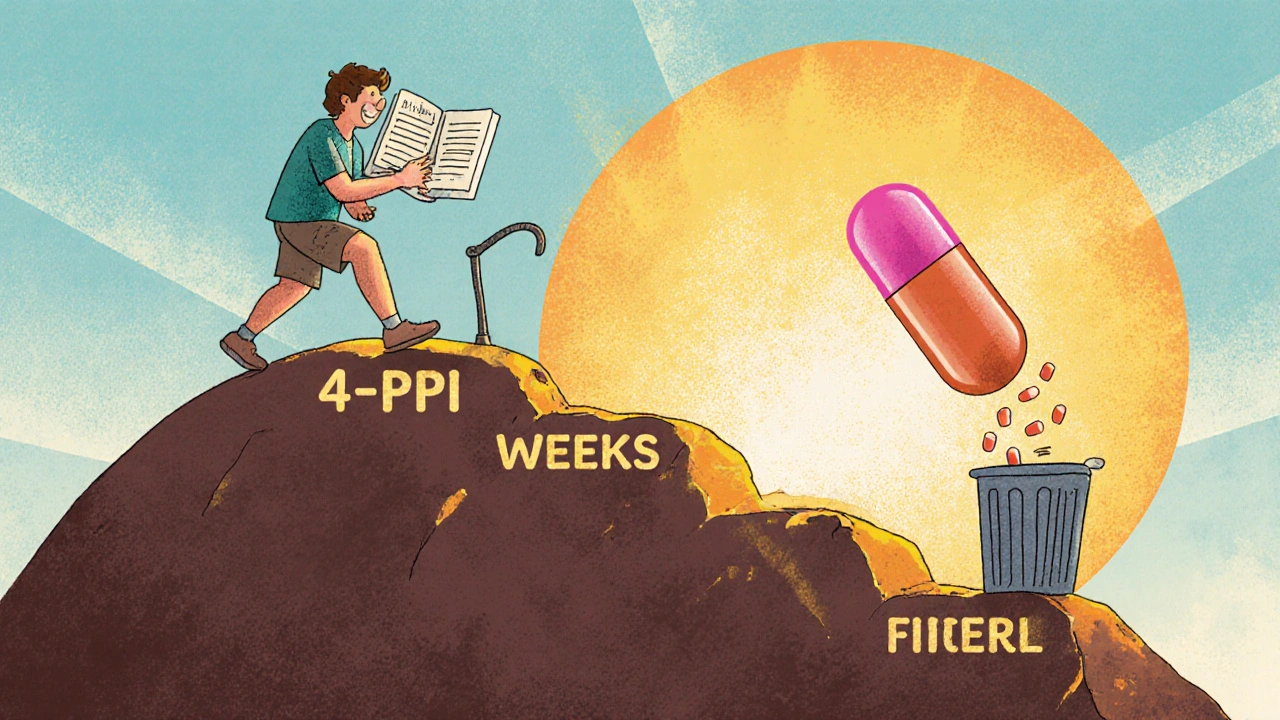
The smartest way to manage GERD isn’t starting with a pill. It’s a step-by-step plan:- Start with lifestyle changes-even if you’re taking PPIs. Weight loss, bedtime fasting, and trigger food avoidance should be your first move.
- Use PPIs only if needed-for moderate to severe symptoms or confirmed esophagitis. Take them correctly: before your first meal.
- Reevaluate after 4-8 weeks. If symptoms are gone, try tapering off. Don’t quit cold turkey. Switch to an H2 blocker for 2 weeks, then stop.
- Use on-demand therapy if symptoms return occasionally. Take a PPI only when you know you’ll eat trigger foods or have a late night.
- Consider alternatives if PPIs fail. New drugs like vonoprazan (Voquezna), approved in 2023, work faster and may be better for some. Endoscopic procedures like LINX® or TIF are options for those who can’t tolerate long-term meds.
When to Worry: Red Flags That Need a Doctor
Not every chest burn is GERD. If you have any of these, see a doctor right away:- Difficulty swallowing (dysphagia)
- Unexplained weight loss
- Vomiting blood or black, tarry stools
- Chronic hoarseness or cough that doesn’t improve
What’s New in 2025?
The field is shifting. The American Gastroenterological Association’s 2024 guidelines now say: Lifestyle changes are the foundation. PPIs are for confirmed damage or severe symptoms. Research from Johns Hopkins showed that a 12-week structured program of diet, sleep elevation, and weight loss allowed 65% of patients to stop PPIs entirely-without symptoms returning. That’s higher than any drug trial. New tech is helping too. Apps like RefluxMD, used by over 8,500 people, track meals and symptoms with 4.7/5 ratings. AI tools are now predicting individual food triggers with 78% accuracy.Final Thought: You Don’t Need to Be on PPIs Forever
Most people can control GERD without lifelong medication. It takes work. It takes patience. But the payoff is huge: no more pills, fewer side effects, and real freedom to eat without fear. Start with one change. Cut out coffee. Don’t eat after 7 p.m. Walk after dinner. Track it. Give it 3 weeks. You might be surprised how much better you feel-even before you touch a pill.Can lifestyle changes cure GERD?
Lifestyle changes don’t always “cure” GERD, but they can eliminate symptoms for many people-especially if the cause is weight, diet, or eating habits. Studies show up to 58% of users achieve moderate to complete control with diet and behavioral changes alone. For others, they reduce the need for medication. The key is consistency and identifying your personal triggers.
How long should I take a PPI?
PPIs are meant for short-term use-typically 4 to 8 weeks for healing. After that, you should reassess. If symptoms are gone, try stepping down to an H2 blocker or stopping entirely. Long-term use (over a year) increases risks like infections, nutrient deficiencies, and bone fractures. Never stay on PPIs longer than needed without medical supervision.
Why do I feel worse when I stop PPIs?
This is called rebound acid hypersecretion. When you take PPIs long-term, your stomach produces more acid-producing cells to compensate. When you stop suddenly, those cells go into overdrive, making acid levels spike. That’s why symptoms return-sometimes worse than before. The fix? Taper slowly. Switch to an H2 blocker like famotidine for 2 weeks, then stop. Don’t quit cold turkey.
Is it safe to take PPIs with other medications?
PPIs can interfere with some drugs. They reduce absorption of iron, vitamin B12, and certain antifungals. They can also increase levels of blood thinners like clopidogrel and reduce the effectiveness of some HIV meds. Always tell your doctor or pharmacist about everything you’re taking-including supplements-before starting a PPI.
What foods should I avoid for GERD?
The biggest triggers are coffee, tomatoes, alcohol, chocolate, fatty or fried foods, spicy foods, citrus, and carbonated drinks. But triggers vary. Keep a food diary for 2-4 weeks. Write down everything you eat and when symptoms happen. You’ll find your own list. For most people, cutting out just coffee and late-night eating makes a huge difference.
Can I still drink alcohol with GERD?
Alcohol relaxes the lower esophageal sphincter and increases stomach acid. Even small amounts can trigger reflux. Wine and beer are common culprits. If you drink, limit it to occasional small servings and never close to bedtime. Many people find they feel better quitting entirely-even if they don’t think alcohol is their trigger.
Should I sleep with my head elevated?
Yes-if nighttime reflux is a problem. Elevating the head of your bed by 6-8 inches uses gravity to keep acid down. Don’t just use extra pillows; that bends your body and can make it worse. Use bed risers or a wedge pillow designed for GERD. Many patients report this single change eliminates nighttime symptoms.
Are there natural remedies that work?
Some people find relief with ginger tea, aloe vera juice, or chewing gum after meals (it boosts saliva, which neutralizes acid). But don’t rely on them alone. No natural remedy reduces acid production like PPIs or H2 blockers. They can help as add-ons-but not replacements-for proven lifestyle and medical strategies.
Next Steps: What to Do Today
If you’re dealing with GERD, here’s your simple action plan:- Start a food and symptom diary for the next 14 days.
- Stop eating at least 3 hours before bed.
- Eliminate coffee and alcohol for 2 weeks.
- If you’re on a PPI, ask your doctor: “Is this still necessary?”
- Try raising the head of your bed if you wake up with heartburn.

Bailey Sheppard
November 18, 2025 AT 23:43Been dealing with this for years. Started with PPIs, then slowly cut back by avoiding coffee and not eating after 7. Didn’t think it would work, but my nights are actually quiet now. No more waking up like I swallowed battery acid.
Girish Pai
November 19, 2025 AT 06:59Western medicine overrelies on PPIs. In Ayurveda, we treat agni imbalance-digestive fire-with triphala, warm water upon waking, and avoiding cold drinks post-meal. No pills needed. The body heals when you stop suppressing and start aligning.
Kristi Joy
November 19, 2025 AT 12:25For anyone feeling overwhelmed-start small. One change. One week. Maybe it’s just not eating in bed. Or drinking water instead of soda at dinner. You don’t have to fix everything at once. Progress isn’t linear, but every step counts. You’ve got this.
Hal Nicholas
November 19, 2025 AT 19:46Everyone’s so eager to ditch PPIs like they’re the devil. Meanwhile, people with erosive esophagitis are still getting endoscopies because they listened to Reddit instead of their GI. You can’t ‘lifestyle’ your way out of a damaged esophagus. Some of us need the meds. Stop pretending otherwise.
Louie Amour
November 21, 2025 AT 06:34Did you know the FDA banned PPIs in 2019? No? Because they didn’t. But the pharmaceutical industry sure loves pushing them. They know if you stop taking them, you’ll need them again. It’s a cash cow. Wake up. The system is rigged. Don’t be a lab rat.
Kristina Williams
November 22, 2025 AT 12:57My cousin took PPIs for 8 years. Then she started drinking apple cider vinegar and now she’s fine. No meds. No doctors. Just vinegar. The whole medical system is built on keeping you sick. They don’t want you cured.
Shilpi Tiwari
November 23, 2025 AT 19:02Interesting data on rebound hypersecretion. The mechanistic basis involves upregulation of H+/K+ ATPase isoforms and increased gastrin secretion via negative feedback loop disruption. However, clinical relevance hinges on individual phenotypic variation in gastric mucosal adaptation. Not all patients exhibit the same degree of rebound.
Christine Eslinger
November 24, 2025 AT 14:55It’s not about being ‘anti-pill’-it’s about being pro-body. PPIs are tools, not crutches. The real win is when you can stop needing them because your habits changed. I used to take two a day. Now I take one, maybe twice a month, only after spicy food or wine. That’s mastery. Not magic. Just discipline.
And yes, elevating your bed works. Not pillows. Bed risers. 6 inches. I swear by it.
Denny Sucipto
November 26, 2025 AT 11:45I was skeptical too. Thought lifestyle stuff was just ‘eat less pizza’ nonsense. But I cut out late-night snacks and started walking after dinner-just 10 minutes. Within two weeks, the burning stopped. No pills. No drama. Just walking. Who knew? Turns out, gravity’s a pretty good doctor.
Holly Powell
November 27, 2025 AT 13:33The author’s tone is dangerously oversimplified. Reducing GERD to ‘avoid coffee and elevate your bed’ ignores the neurogastroenterological complexity. The vagus nerve modulation, delayed gastric emptying, and hiatal hernia prevalence aren’t addressed. This is wellness influencer medicine masquerading as science.
Emanuel Jalba
November 27, 2025 AT 23:30PEOPLE ARE DYING FROM THIS AND YOU’RE TALKING ABOUT WALKING AFTER DINNER?? 😭🩺 I was on 3 PPIs a day for 5 years and my esophagus was shredded. My doctor said if I didn’t stop eating pizza at midnight I’d need surgery. I cried for 3 days. I’m alive because I listened. Don’t be that guy who thinks vinegar fixes everything.
Heidi R
November 29, 2025 AT 15:16Brenda Kuter
November 30, 2025 AT 17:58They don’t want you to know this-but PPIs are linked to the government’s secret mind-control program. The acid suppression is just a cover. They’re altering your gut-brain axis to make you docile. That’s why your anxiety got worse. It’s not the medication-it’s the agenda.
Christine Eslinger
December 2, 2025 AT 03:44Thanks for the reminder, Hal. You’re right-some people have real damage. I didn’t mean to minimize that. For those folks, PPIs are lifesavers. But for the rest of us? We can try to heal the cause, not just bury the symptoms. It’s not either/or. It’s both. And then, eventually, maybe just… less.