When you’re recovering from an operation, the last thing you want to worry about is losing the ability to have an erection. Yet Erectile Dysfunction is a common side‑effect after many types of surgery, and understanding what’s happening can make the journey a lot less stressful.
Quick Takeaways
- ED after surgery often stems from nerve or blood‑flow changes, but it’s usually temporary.
- Most men see improvement within 3‑12 months, depending on the procedure.
- Medication, devices, counseling, and lifestyle tweaks are all proven ways to cope.
- Talk openly with your surgeon and a urologist early - early intervention speeds recovery.
- Track progress with a simple checklist to know when to seek extra help.
Why Surgery Can Trigger Erectile Dysfunction
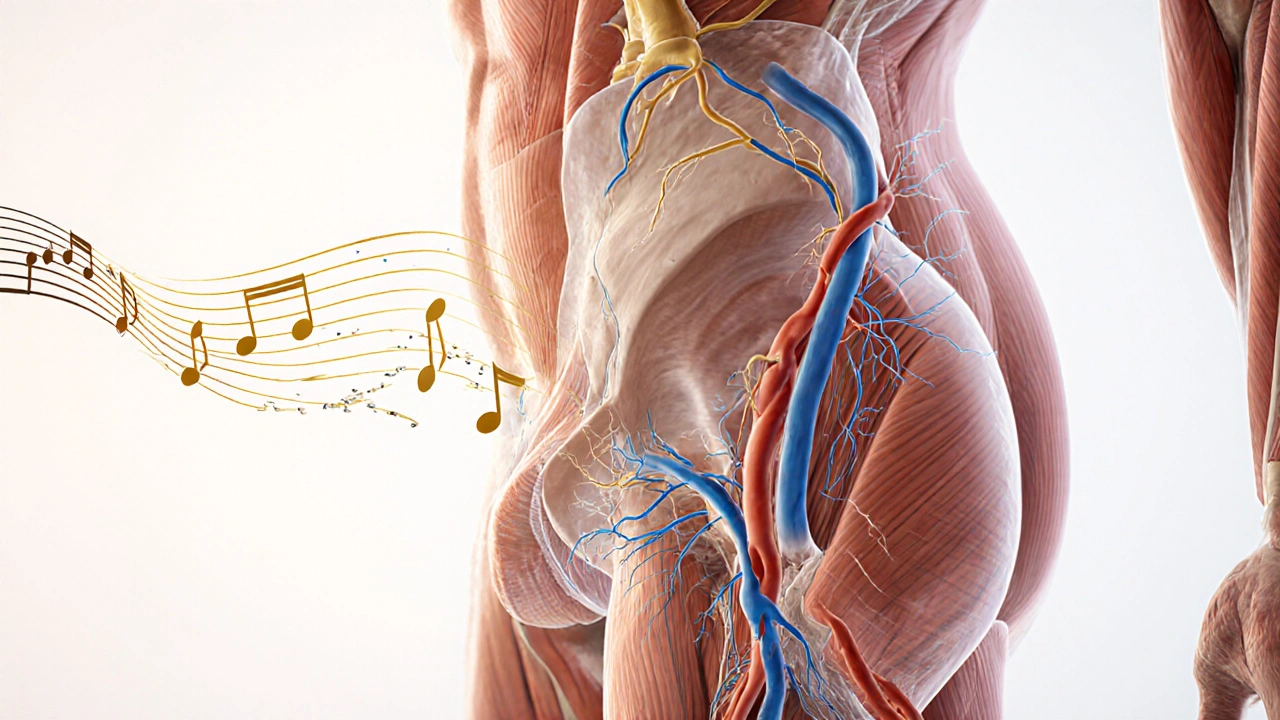
During many operations, especially those near the pelvis or spine, surgeons may unintentionally affect the nerves, blood vessels, or hormones that control an erection. Think of an erection like a well‑orchestrated concert: nerves send the signal, blood vessels deliver the flow, and hormones keep the rhythm. If any instrument is out of tune, the performance suffers.
Nerve Damage is the most common culprit. Procedures such as radical prostatectomy, bladder removal, or colorectal surgery can stretch or cut the cavernous nerves that trigger blood flow. Even non‑pelvic surgeries - like certain cardiac or orthopedic operations - can cause temporary nerve irritation.
Blood‑Flow Disruption occurs when vessels are clamped, scar tissue forms, or medications affect circulation. If the penile arteries can’t fill properly, an erection won’t happen.
Finally, Psychological Factors such as anxiety, depression, or fear of pain often add a mental block. The mind and body are tightly linked, so stress about recovery can amplify physical issues.
Surgeries Most Often Linked to Post‑Operative ED
Not every operation carries the same risk. Here are the big three that doctors cite most often:
- Radical Prostatectomy - removal of the prostate for cancer. Nerve‑sparing techniques have improved outcomes, but up to 40% of men still notice some degree of ED in the first year.
- Rectal or Colon Resection - especially low anterior resections. Proximity to pelvic nerves can cause temporary or lasting erectile issues.
- Spinal Surgery - especially procedures involving the lower thoracic or lumbar spine. Direct nerve contact can affect the signal pathway.
Other surgeries - such as major cardiac bypass, hip replacements, or extensive abdominal procedures - can also lead to postoperative ED, though the rates are lower.
What the Recovery Timeline Looks Like
Every man’s healing curve is unique, but most follow a similar pattern:
- First 4‑6 weeks: Swelling, pain, and limited activity dominate. Nerve irritation is at its peak, so erections are often weak or absent.
- 6‑12 weeks: Nerves start to regenerate (about 1mm per day). You may notice occasional “nighttime” erections, a good sign that the pathway is re‑establishing.
- 3‑6 months: Many men report noticeable improvement, especially if they’re using medication or devices.
- 6‑12 months: Full nerve recovery, if it’s going to happen, is usually evident. Persistent problems after a year merit specialist evaluation.
If you’re past 12 months and still struggling, don’t assume it’s permanent - new therapies and surgical revisions can help.

Physical Coping Options
When you’re ready to act, there are several proven treatments. Below is a quick rundown of the most common choices.
| Option | How It Works | Typical Onset | Pros | Cons |
|---|---|---|---|---|
| PDE5 Inhibitors (e.g., Viagra, Cialis) | Enhances nitric‑oxide signaling to improve blood flow. | 30‑60minutes | Oral, easy, works for many. | May not work if nerves are severely damaged; side‑effects like headache. |
| Vacuum Erection Device (VED) | Creates suction, drawing blood into the penis. | Immediate | Non‑invasive, useful for early recovery. | Requires manual effort; may feel unnatural. |
| Penile Implant | Surgical rods that provide rigidity. | Weeks after surgery | Highest satisfaction for severe cases. | Invasive, higher cost, requires surgery. |
| Intracavernosal Injections | Directly inject vasodilator into the penis. | 5‑15minutes | Effective when pills fail. | Needle anxiety; risk of priapism. |
Most doctors start with PDE5 inhibitors because they’re simple. If you’re within the first three months post‑op, a Vacuum Erection Device can keep the tissue healthy and prevent fibrosis.
Psychological Coping Strategies
Even if the physical cause is clear, the mental side can linger. Here’s how to keep the mind in the game:
- Sexual Counseling - A therapist trained in sexual health helps you and your partner talk about expectations, reducing performance anxiety.
- Mindfulness & Relaxation - Simple breathing exercises or guided meditations can lower stress hormones that hinder blood flow.
- Open Communication - Let your partner know what you’re feeling. Most couples discover that honesty actually improves intimacy.
Studies from the American Urological Association show that men who combine medication with counseling report a 20% higher satisfaction rate than medication alone.
Lifestyle Tweaks That Speed Recovery
What you eat, how you move, and what you avoid can tip the balance toward healing.
- Exercise - Light cardio (30min, 4‑5×/week) boosts circulation. Pelvic floor (Kegel) exercises strengthen the muscles that help retain blood.
- Nutrition - Foods rich in antioxidants (berries, leafy greens) and omega‑3s (salmon, walnuts) support nerve repair.
- Avoid Smoking & Excess Alcohol - Both constrict vessels and delay nerve regeneration.
- Weight Management - Obesity raises the risk of persistent ED by up to 30%.
Even small changes-like swapping a nightly beer for a glass of water-can add up. Keep a simple diary for a month to see which habits make the biggest difference.
Checklist: What to Discuss With Your Surgeon or Urologist
- Type of surgery performed and whether nerve‑sparing techniques were used.
- Timeline of any erections you’ve noticed (nighttime, morning, with medication).
- Current medications (including pain meds that may affect libido).
- Interest in trying PDE5 inhibitors, VEDs, or other options.
- Whether you’ve spoken with a mental‑health professional about anxiety.
- Lifestyle factors-smoking, alcohol, activity level.
Having this list ready makes the appointment efficient and shows you’re proactive.
When to Seek Additional Help
Most men improve within a year, but there are signals that warrant a deeper dive:
- No erections at all after 6months, even with medication.
- Painful erections (priapism) or severe curvature.
- Significant emotional distress, depression, or relationship strain.
- Underlying conditions like diabetes that could compound the issue.
If any of these apply, ask for a referral to a specialized erectile dysfunction clinic. They can run Doppler ultrasound tests to assess blood flow and nerve function, then tailor a treatment plan.
Frequently Asked Questions
How long does it usually take for erections to return after prostate surgery?
Most men see some improvement between 3 and 9 months, but full recovery can take up to 18 months. Nerve‑sparing techniques improve odds, and using a vacuum device early on helps keep tissue healthy.
Can I use Viagra right after surgery?
It’s safe for most men, but you should wait until your surgeon clears you-usually after the first two weeks when wound healing is stable. Starting low (25mg) and monitoring blood pressure is wise.
Are there non‑medication options that work?
Yes. Vacuum erection devices, pelvic floor exercises, and counseling can all improve function, especially in the early recovery phase.
What if my partner feels pressured or worried?
Open communication is key. Invite your partner to appointments, discuss coping strategies together, and consider joint counseling. Shared understanding lowers anxiety for both.
Is penile implant a last‑resort option?
Implants are generally considered when medication and devices have failed after at least 12 months of trying. Success rates exceed 90% in satisfied patients, but the decision involves surgery and recovery time.
Next Steps for Your Recovery Journey
1. **Schedule a follow‑up** with your surgeon or a urologist within the next two weeks. 2. **Start a simple log**: note any erections, medications taken, and mood each day. 3. **Pick a coping method** - trial a PDE5 inhibitor or a vacuum device as advised. 4. **Add a daily habit** - 20‑minute walk and a short pelvic‑floor routine. 5. **Talk to your partner** - share the plan, ask for support, and consider a joint counseling session.
Recovering from post‑surgery erectile dysfunction isn’t a race; it’s a steady, step‑by‑step process. By understanding the why, setting realistic expectations, and using the tools outlined here, you give yourself the best shot at getting back to a satisfying sex life.
Kyle Salisbury
October 10, 2025 AT 19:56Hey folks, just wanted to say that this guide does a solid job of breaking down a tough subject. It’s important to remember that post‑surgery ED is usually temporary and that open dialogue with your doctor can make a huge difference. I’ve seen patients who keep a simple log of their erections and meds feel more empowered during follow‑up visits. Also, don’t underestimate the power of small lifestyle tweaks – a walk around the block or a handful of berries can actually support nerve healing.
Patrick Rauls
October 20, 2025 AT 02:15Totally agree!! 😊 Keep that diary and the meds, the VED is a game‑changer early on. Don’t be shy about asking the doc for a low‑dose pill first – better safe than sorry.
Keri Shrable
October 29, 2025 AT 07:34Wow, love the colorful breakdown! 🌈 It’s nice to see the mix of physical and mental tips – especially the part about mindfulness. I always tell my buddies that a calm mind can actually boost blood flow. Keep the optimism flowing, guys!
Destiny Hixon
November 7, 2025 AT 13:52Look, all that feel‑good stuff is nice but you gotta remember that if the nerves are ripped the meds won’t help much. Don’t waste time with fancy gadgets until the doctor says it’s safe. Real talk – put the effort in rehab first.
mike brown
November 16, 2025 AT 20:11Honestly, I think this whole "just wait" narrative is over‑hyped. Sure, some recover, but many end up stuck and the guide barely mentions the cost of implants. If you’re not seeing progress by six months, maybe push for more aggressive treatment sooner.
shawn micheal
November 26, 2025 AT 02:30Hey, I hear you, mike. It’s true that waiting can be frustrating, but jumping straight to surgery isn’t always the answer. A graduated plan – start with low‑dose PDE5 inhibitors, add a vacuum device, and keep a log – often yields progress without the high price tag of implants.
Stephen Jahl
December 5, 2025 AT 08:49From a clinical perspective, the pathophysiology of postoperative erectile dysfunction can be delineated into three principal domains: neurogenic disruption, vascular compromise, and psychogenic inhibition. Neurogenic injury, particularly to the cavernous nerves, precipitates an immediate diminution in nitric oxide synthesis, thereby attenuating smooth muscle relaxation within the corpora cavernosa. This loss of neurogenic tone is quantifiable via nocturnal penile tumescence testing, which frequently reveals a marked reduction in rigidity epochs during the early postoperative window. Concurrently, vascular insult-whether iatrogenic arteriolar spasm or postoperative edema-exacerbates the hemodynamic insufficiency requisite for erection. The intricate interplay between these mechanisms manifests clinically as a spectrum of erectile potency ranging from occasional nocturnal erections to complete anorgasmia. Empirical data suggest that a majority of patients experience modest improvement within the 3‑ to 6‑month interval, contingent upon the presence of nerve‑sparing surgical techniques; however, this recovery trajectory is highly variable and subject to comorbid conditions such as diabetes mellitus and peripheral vascular disease. Pharmacologic adjuncts, most notably phosphodiesterase‑type 5 inhibitors, augment cyclic guanosine monophosphate concentrations, thereby partially compensating for impaired neuronal input. Their efficacy, however, is predicated upon sufficient residual endothelial function, rendering them suboptimal in cases of severe neurovascular damage. In such scenarios, mechanical modalities, including vacuum erection devices, serve to preserve corporal tissue elasticity and mitigate fibrosis, a critical consideration given the propensity for fibroelastic remodeling in the chronic post‑operative milieu. Intracavernosal injection therapy, employing agents such as alprostadil, provides a direct pharmacodynamic bypass of neurogenic pathways, affording reliable tumescence albeit with an elevated risk of priapism. When conservative measures prove insufficient, penile prosthesis implantation remains the definitive therapeutic recourse, boasting satisfaction rates exceeding 90% in appropriately selected cohorts. Nonetheless, the decision to proceed with prosthetic surgery must be juxtaposed against the inherent operative risks and the psychological implications of a permanent implant. It is incumbent upon clinicians to adopt a multidisciplinary approach, integrating urologic expertise, psychosexual counseling, and rehabilitative physiotherapy to optimize functional outcomes. Regular follow‑up appointments, bolstered by objective metrics such as duplex ultrasonography, facilitate timely identification of suboptimal recovery patterns and enable iteration of the therapeutic algorithm. Ultimately, patient education regarding the anticipated timeline and therapeutic arsenal is paramount to ameliorating anxiety and fostering adherence to the prescribed regimen.
gershwin mkhatshwa
December 14, 2025 AT 15:08That was a marathon of a post, Stephen! 👍 I think the key takeaway is balance – meds, devices, and mindset all play a role. Remember to keep the pelvic floor muscles active; those Kegels aren’t just for women. Also, a buddy system with your partner can turn the whole process into a teamwork thing rather than a solo struggle.
Louis Robert
December 23, 2025 AT 21:27Keep a daily log – it works.
tim jeurissen
January 2, 2026 AT 03:46While the guide is comprehensive, it occasionally suffers from imprecise terminology – for instance, conflating "nerve‑sparing" with "nerve‑preserving" which are not synonymous. Moreover, the omission of the term "vasculogenic" when discussing blood‑flow disruption undermines the nuance required for a truly scholarly exposition. Precision in language begets precision in treatment.
lorna Rickwood
January 11, 2026 AT 10:05Yo tim i get u but sometimes u nedd 2 let peeps breath a lil’ i mean its a guide not a thesis lol
Mayra Oto
January 20, 2026 AT 16:24Glad to see such a thorough overview. Sharing cultural perspectives can really help normalize these conversations, especially in communities where talking about sexual health is still a taboo.
S. Davidson
January 29, 2026 AT 22:43Look, I don’t mean to be harsh, but the checklist at the end is basically a copy‑paste from every urology textbook out there. If you’re serious about helping patients, you need original insights, not just rehashed bullet points.
Haley Porter
February 8, 2026 AT 05:02Philosophically, erectile function can be viewed as an emergent property of the interplay between somatic autonomy and relational synchrony. When surgical trauma perturbs this delicate equilibrium, the resulting dysfunction is not merely a physiologic deficit but a phenomenological dissonance that reverberates through one’s sense of self. Re‑establishing that harmony requires both biomedical intervention and a reconstruction of narrative identity.
Samantha Kolkowski
February 17, 2026 AT 11:21Interesting take, Haley. I’d add that the social component-how partners react and support-can be just as critical as the meds. A compassionate partner can help re‑wire those neural pathways through positive reinforcement.
Gauri Omar
February 26, 2026 AT 17:40Let me paint a picture: a man emerges from the operating theater, his body bruised, his pride shattered, and the very act that defined his masculinity feels like a distant memory. The anguish is not just physical; it’s an existential storm that threatens to drown his very sense of worth. Yet, within this darkness, there lies a flicker of hope-science, love, and perseverance can together forge a new dawn.