Stress Impact Assessment
Answer these questions to understand your personal stress-related weight patterns and get customized recommendations based on your lifestyle.
Your Tailored Coping Strategies
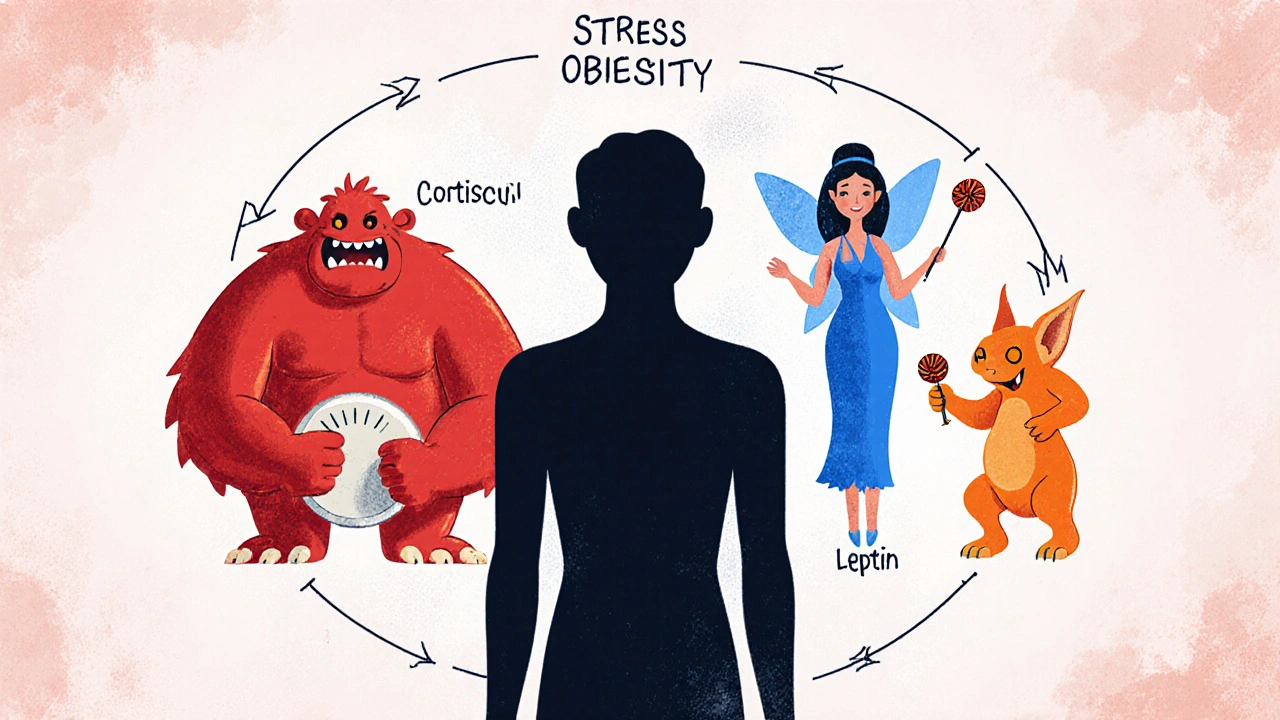
When Stress is the body’s response to perceived threats or pressures, triggering hormonal and behavioral changes collides with Obesity a chronic condition marked by excess body fat that raises health risks, the result is often unwanted stress obesity and stubborn weight gain. Understanding how these two forces interact helps you break the cycle before the scale moves further.
Why Stress Drives Weight Gain
Stress activates the hypothalamic‑pituitary‑adrenal (HPA) axis, flooding the bloodstream with cortisol. While cortisol helps you cope in the short term, chronic elevation nudges the body toward energy storage. It pushes glucose into the bloodstream, spikes insulin, and tells the brain that you need to keep the extra calories “just in case.” Over months, this metabolic shift translates into more fat, especially around the abdomen.
Beyond hormones, stress hijacks decision‑making centers in the brain. The prefrontal cortex, which governs self‑control, gets suppressed, while the amygdala - the fear centre - becomes overactive. The net effect? Cravings for quick‑energy foods, lower motivation to move, and a tendency to skip sleep.
Hormonal Messengers: Cortisol, Leptin, and Ghrelin
Cortisol is a glucocorticoid hormone released during stress that regulates metabolism and immune response isn’t the only player. Two appetite hormones - Leptin signals satiety to the brain and helps regulate energy balance and Ghrelin stimulates hunger and promotes food intake - become dysregulated under chronic stress.
- Elevated cortisol blunts leptin sensitivity, so you feel less full even after eating.
- Stress spikes ghrelin, especially at night, leading to late‑night snacking.
- The imbalance creates a feedback loop: more eating, more fat, more leptin resistance.
Metabolic Side Effects: Insulin Resistance & Fat Storage
Insulin resistance occurs when cells respond poorly to insulin, causing higher blood sugar levels and increased fat storage is a frequent companion of chronic stress. When cortisol forces the liver to release extra glucose, insulin works overtime. Over time, cells down‑regulate insulin receptors, and the body starts storing more of the excess glucose as visceral fat.
This metabolic state not only adds pounds but also raises the risk of type‑2 diabetes, heart disease, and fatty liver. The good news is that improving insulin sensitivity can be tackled with simple lifestyle tweaks - a topic we’ll cover in the coping section.
Behavioural Pathways: Emotional Eating & the Gut Microbiome
When emotions run high, many turn to food for comfort. This pattern, known as Emotional eating refers to consuming food in response to feelings rather than hunger, often involves high‑sugar, high‑fat snacks that spike dopamine and temporarily soothe stress. Unfortunately, the relief is fleeting and the calories add up.
Stress also reshapes the Gut microbiome the community of trillions of bacteria living in the digestive tract that influence digestion, immunity, and mood. A stressed gut tends to host fewer beneficial bacteria (like Bifidobacteria) and more inflammatory strains, which can worsen insulin resistance and trigger cravings for processed carbs.
Sleep & Activity: The Missing Links
Sleep quality refers to how restorative and uninterrupted a night's rest is, influencing hormone balance and cognitive function is a silent driver of weight gain. Poor sleep raises ghrelin, lowers leptin, and leaves you feeling lethargic, making exercise feel like a chore.
Conversely, regular Physical activity includes any movement that raises heart rate and burns calories, from walking to high‑intensity interval training acts as a natural stress buffer. Exercise reduces cortisol, improves insulin sensitivity, and releases endorphins that lift mood without extra calories.

Practical Coping Strategies
Below is a step‑by‑step toolkit you can start using today. Each item tackles a different piece of the stress‑obesity puzzle.
- Track stress triggers. Keep a simple journal - note the time of day, situation, and mood before you eat. Patterns reveal the true culprits.
- Master quick breathing. The 4‑7‑8 technique (inhale 4 seconds, hold 7, exhale 8) lowers cortisol within minutes and curbs impulse bites.
- Eat protein at each meal. Protein stabilizes blood sugar, keeps leptin signaling strong, and reduces cravings for sugary snacks.
- Swap sugary comfort foods for fiber‑rich alternatives. A handful of berries with Greek yogurt satisfies sweet cravings while feeding good gut bacteria.
- Schedule movement. Aim for 30 minutes of moderate activity most days. Even a brisk walk after a stressful meeting can reset hormone levels.
- Prioritise sleep hygiene. Darken the bedroom, limit screens an hour before bed, and keep a consistent bedtime to normalize ghrelin and leptin.
- Practice mindful eating. Put the fork down between bites, chew slowly, and ask yourself if you’re truly hungry or just stressed.
- Consider professional support. A therapist trained in cognitive‑behavioral stress management or a dietitian familiar with stress‑related eating can provide personalized strategies.
Quick Checklist for Managing Stress‑Related Weight Gain
- Identify three top stress triggers each week.
- Do a 4‑7‑8 breathing session before any snack.
- Include a source of lean protein at every meal.
- Swap one processed snack per day for a whole‑food alternative.
- Move for at least 20 minutes after each stressful event.
- Set a consistent bedtime and wake‑up time.
- Use a journal to log hunger vs. emotional urges.
- Book a consultation with a health professional if patterns persist.
Frequently Asked Questions
Can occasional stress cause weight gain?
Short‑term spikes in cortisol may lead to temporary water retention and a slight increase in appetite, but lasting weight gain usually requires chronic stress combined with poor eating habits.
Is cortisol the only hormone involved?
No. Leptin, ghrelin, insulin, and adrenaline also shift during stress, influencing hunger, satiety, and how the body stores fat.
How much sleep do I need to keep hormones balanced?
Most adults benefit from 7‑9 hours of uninterrupted sleep. Consistently getting less than 6 hours raises ghrelin and lowers leptin, making cravings more likely.
Will exercise completely offset stress‑induced cortisol?
Exercise reduces cortisol over the long term and improves insulin sensitivity, but it works best alongside other stress‑management practices like breathing or meditation.
Is there a specific diet that counters stress‑related weight gain?
A balanced diet rich in lean protein, fiber, healthy fats, and low‑glycemic carbs helps stabilise blood sugar, supports gut health, and keeps hormone levels steadier.

Dan Danuts
October 23, 2025 AT 17:05Great overview! I love how you break down the cortisol‑ghrelin loop and give practical steps. I’ve started the 4‑7‑8 breathing before late‑night snacks and notice I’m less likely to raid the pantry. Keep sharing these easy hacks!
Dante Russello
November 4, 2025 AT 05:51Your post hits the nail on the head; stress really does hijack our metabolism, and the cascade you described is spot‑on. First, the HPA axis fires up cortisol, which in turn pushes glucose into the bloodstream, prompting the pancreas to release insulin; over time this repetitive surge wears down insulin receptors. Second, you mentioned leptin resistance-this is crucial because when leptin can’t signal satiety properly, we keep eating even when the body is full. Third, the ghrelin spikes at night explain those stubborn cravings for cookies after a long day; I’ve personally felt that after a stressful meeting. Fourth, the gut microbiome shift you highlighted adds another layer; fewer Bifidobacteria means more inflammation and more sugar cravings. Fifth, lack of sleep compounds the whole problem by raising ghrelin and dropping leptin, turning a simple snack into a calorie bomb. Sixth, regular movement acts as a natural buffer; even a brisk 20‑minute walk can lower cortisol levels within an hour. Seventh, mindful eating-putting the fork down between bites-helps reset the brain’s reward pathways, and prevents emotional eating loops. Eighth, journaling stress triggers, as you suggested, is a low‑cost but high‑return strategy; patterns become visible, and you can intervene before the habit solidifies. Ninth, protein at every meal stabilizes blood sugar, keeping cravings at bay, and also supports muscle maintenance while you’re cutting weight. Tenth, swapping sugary treats for fiber‑rich options feeds good gut bacteria, which in turn supports better mood and metabolic health. Eleventh, consistent sleep hygiene-dark room, no screens-helps normalize hormone rhythms, and you’ll notice better energy for workouts. Twelfth, consider professional help if the cycle feels unbreakable; a therapist can teach cognitive‑behavioral techniques that directly target stress‑induced eating. Thirteenth, staying hydrated is often overlooked; sometimes thirst masquerades as hunger. Fourteenth, supplementing with omega‑3 fatty acids can reduce inflammation and improve insulin sensitivity. Finally, remember that stress is inevitable, but the tools you choose to manage it determine whether you gain weight or stay on track. Awesome guide!
James Gray
November 15, 2025 AT 19:38Man, that was a solid breakdown, I vibed with the part about journaling stress triggers. I’ve started write down my mood before dinner and it's crazy how often I catch myself reaching for chips. The 4‑7‑8 breathing is simple, I do it in the office and feel the tension melt away. Keep dropping these gems, they really help us level up our health game. Thanks for the science and the practical tips!
Scott Ring
November 27, 2025 AT 09:25I appreciate how the article links hormonal changes to everyday habits. It reminds us that cultural food choices can either fuel or fight stress‑related cravings. Integrating traditional herbs that support cortisol balance can be a great addition to the toolkit.
Shubhi Sahni
December 8, 2025 AT 23:11Exactly! Adding spices like turmeric or ashwagandha not only honors cultural traditions, but also helps modulate cortisol levels, which can curb those stress‑induced snack attacks. Consistency is key-making these additions a daily habit amplifies the benefits. Glad you highlighted this angle!
Danielle St. Marie
December 20, 2025 AT 12:58Honestly, most people just use excuses for their weight gain-stress is a convenient scapegoat. 💪 If you want results, stop whining and start disciplined action. 🏋️♀️ No one’s going to fix your hormones while you sit on the couch binge‑watching. 🚫
keerthi yeligay
January 1, 2026 AT 02:45So true, stress eats you from inside.
Peter Richmond
January 12, 2026 AT 16:31While accountability is essential, it is equally important to recognize the physiological impact of chronic stress on metabolism.
Bonnie Lin
January 24, 2026 AT 06:18Thanks for the thorough guide. These steps are realistic and easy to fit into a busy schedule. I’ll try the protein‑every‑meal tip next week.