Eye Pressure Myth vs. Fact Checker
Test your understanding of common eye pressure myths and facts. Select the correct answer for each statement below.
Many people believe that glaucoma only develops when eye pressure exceeds 30 mmHg.
Some believe that low eye pressure is always safe and harmless.
Eye pressure changes are usually painless, so symptoms are rare.
IOP naturally fluctuates throughout the day due to various factors.
Different tonometry techniques vary in accuracy and use cases.
Juvenile forms of glaucoma can occur in children and young adults.
Several treatment options exist beyond eye drops for managing IOP.
Elevated IOP is a risk factor but not a certainty for vision loss.
Physical activity and dietary choices can impact IOP levels.
Glaucoma is a chronic condition requiring lifelong management.
Your Results Summary
Complete all questions to see your score and summary.
When you hear the phrase eye pressure myths, you probably picture vague warnings about blurry sight or scary warnings about permanent blindness. The truth is, many of those warnings are either exaggerated or flat‑out wrong. Below we pull apart the ten most common misconceptions, give you the science behind each, and show you what really matters for protecting your eyes.
What Is Eye Pressure, Anyway?
In medical terms, eye pressure is called Intraocular Pressure (IOP) - the fluid pressure inside the eye that helps maintain its shape and proper optical function. IOP is measured in millimeters of mercury (mmHg) and normally ranges between 10 and 21 mmHg. The pressure is created by the continuous production and drainage of a clear fluid called aqueous humor.
Myth #1: Only High Pressure Causes Glaucoma
Many people think glaucoma only shows up when IOP shoots above 30mmHg. In reality, normal‑tension glaucoma exists - that’s when optic nerve damage occurs even though pressure stays within the “normal” range. Glaucoma - a group of eye diseases that damage the optic nerve - can develop at any pressure level, especially if blood flow to the nerve is compromised. Regular eye exams are the only way to catch early signs.
Myth #2: Low Pressure Means No Risk
Conversely, some hear that low IOP rules out any danger. Low pressure (hypotony) can actually indicate a leak in the eye’s drainage system or an eye injury, both of which can threaten vision. While low pressure rarely leads to glaucoma, it still warrants a professional evaluation.
Myth #3: Eye Pressure Is Only Checked When You Have Symptoms
Eye pressure changes are usually painless, so you won’t feel a headache, ache, or any other warning sign. That’s why tonometry - the test that measures IOP - is part of a routine comprehensive eye exam. Even if you think your eyes are fine, an annual check can spot problems early.
Myth #4: Eye Pressure Stays the Same All Day
IOP fluctuates naturally throughout the day, typically peaking in the early morning and dipping in the evening. Factors like caffeine, stress, and even body position can cause short‑term spikes. If your doctor suspects glaucoma, they may recommend multiple measurements at different times to get an accurate picture.
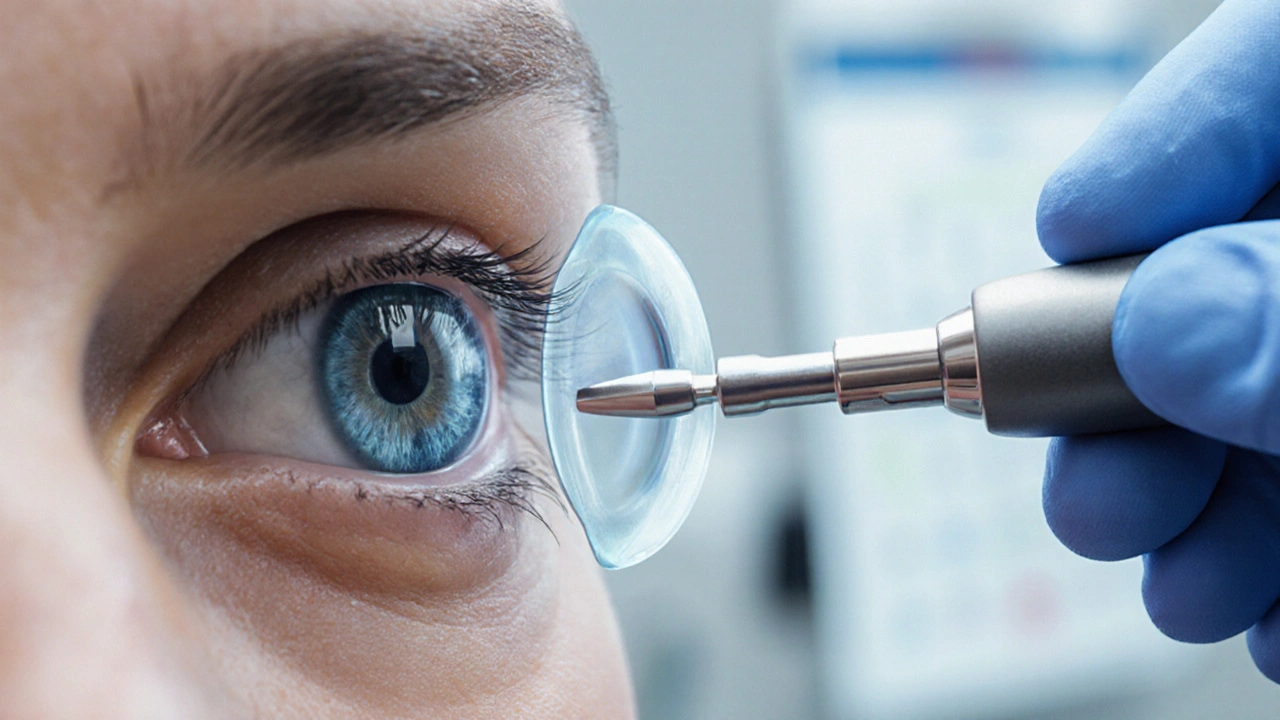
Myth #5: All Tonometry Methods Are Identical
There are several ways to measure IOP, each with pros and cons. The classic Goldmann Applanation Tonometer - a small probe that gently flattens a part of the cornea - is still the gold standard for accuracy. Non‑contact (air puff) tonometry uses a puff of air and is quick but can be less precise. A newer trend is hand‑held portable devices that allow quick screening in community settings.
Myth #6: If You’re Young, You Don’t Need to Worry About IOP
While glaucoma is more common after age 40, juvenile forms do exist. Certain genetic conditions, eye injuries, or steroid use can raise IOP in younger patients. If a family member has glaucoma, a pediatric ophthalmologist may start monitoring early.
Myth #7: Eye Drops Are the Only Way to Lower Pressure
Medication is often the first line of treatment, but laser therapy (such as selective laser trabeculoplasty) and surgical options (like trabeculectomy or minimally invasive glaucoma surgery) can effectively reduce IOP when drops aren’t enough or cause side effects.
Myth #8: High Eye Pressure Guarantees Vision Loss
Elevated IOP is a risk factor, not a guarantee. Some people with chronically high pressure never develop optic nerve damage, while others with modest elevations suffer serious loss. The key is regular monitoring of both pressure and optic nerve health.
Myth #9: Lifestyle Doesn’t Influence Eye Pressure
Research shows that regular aerobic exercise can modestly lower IOP - typically a drop of 1-2mmHg after a brisk walk. Conversely, activities that sharply raise blood pressure, like heavy weightlifting, may cause temporary spikes. Maintaining a healthy weight and limiting caffeine can also help keep pressure stable.

Myth #10: Once Treated, IOP Stays Stable Forever
Glaucoma is a chronic condition. Even after successful surgery or laser treatment, IOP can rise again over months or years. Lifelong follow‑up with an ophthalmologist - a medical doctor specializing in eye diseases - is essential to adjust treatment as needed.
Quick Myth‑Fact Comparison
| Myth | Fact |
|---|---|
| Only high pressure causes glaucoma | Glaucoma can occur at normal or low pressures. |
| Low pressure is harmless | Very low pressure can signal eye injury or leakage. |
| You feel symptoms before damage | IOP changes are usually painless; routine checks are needed. |
| Pressure is constant all day | IOP fluctuates with time of day and activities. |
| All tonometers give the same reading | Methods vary in precision; Goldmann remains the gold standard. |
| Only seniors need monitoring | Juvenile glaucoma exists; family history matters. |
| Eye drops are the only treatment | Laser and minimally invasive surgery are effective alternatives. |
| High pressure always leads to vision loss | Many with high IOP never develop optic damage. |
| Lifestyle has no effect | Aerobic exercise can lower IOP; certain activities cause spikes. |
| One treatment cures IOP forever | Glaucoma requires lifelong monitoring and possible adjustments. |
How to Take Action Today
- Schedule a comprehensive eye exam that includes IOP measurement, especially if you’re over 40 or have a family history of glaucoma.
- Ask your eye doctor which tonometry method they use and why.
- If prescribed eye drops, follow the regimen exactly and report any side effects.
- Incorporate moderate aerobic exercise (e.g., 30 minutes of brisk walking) most days of the week.
- Limit caffeine intake to 1-2 cups per day and avoid smoking.
- Stay informed about new treatment options - laser and MIGS procedures are becoming more common.
Common Follow‑Up Questions
Frequently Asked Questions
How often should I get my eye pressure checked?
If you’re over 40 or have risk factors, an annual check is recommended. Those with known glaucoma may need checks every 3-6 months.
Can I measure my eye pressure at home?
Home tonometry devices exist, but they are not as accurate as clinic equipment. Use them only under a doctor’s guidance and confirm results at a professional exam.
What are the side effects of glaucoma eye drops?
Common issues include a stinging sensation, blurry vision, or changes in eye color (with certain prostaglandin analogs). Your ophthalmologist can adjust the formula if needed.
Is laser treatment painful?
Laser trabeculoplasty is usually done under a numbing eye drop. Most patients feel only a brief flashing sensation and recover quickly.
Can diet affect eye pressure?
A diet rich in leafy greens, omega‑3 fatty acids, and low in sodium may support overall eye health, though direct impact on IOP is modest compared to medication and exercise.
Val Vaden
October 7, 2025 AT 17:13Wow, another boring eye‑pressure list 🙄.
lalitha vadlamani
October 7, 2025 AT 20:00It is disheartening to witness the proliferation of misinformation regarding ocular health, especially when such fallacies jeopardize public well‑being. One must acknowledge the moral responsibility of disseminating accurate scientific data, lest we become complicit in needless suffering. The author’s effort to debunk myths is commendable, yet the presentation borders on the pedantic, sacrificing clarity for verbosity. I implore readers to reflect upon the gravity of eye‑pressure neglect and to prioritize regular examinations. Let us not be swayed by complacency, for the cost of blindness is far too dear.
kirk lapan
October 8, 2025 AT 00:10Alright, let me lay it out piece by piece, because the average joe on reddit seems to think "glaucoma" is just a fancy word for bad eyesight, which is totally wrong. First off, intraocular pressure (IOP) ain't just some static number you can read off a gauge and forget about; it fluctuates like my mood on a Monday morning. Second, the myth that only high pressure causes glaucoma is a classic case of oversimplification – normal‑tension glaucoma exists and can silently chew up the optic nerve while your pressure reads "perfectly fine". Third, low pressure is not a free pass – hypotony can signal a leak or trauma, and that’s a red flag you don’t want to ignore.
Now, about the testing: tonometry methods differ, and the Goldmann applanation tonometer is still the gold standard, not some cheap air‑puff gizmo you see at a drugstore. Fourth, you can’t rely on symptoms because IOP changes are usually painless – that’s why routine exams are essential.
Fifth, the idea that pressure stays constant all day is nonsense. It peaks in the early morning, dips later, and can be nudged up by caffeine, stress, even heavy lifting. Sixth, youth is not an immunity shield – juvenile glaucoma is a thing, especially if there’s a family history or steroid use.
Seventh, eye drops are not the sole treatment; laser trabeculoplasty and minimally invasive surgeries (MIGS) can be equally effective. Eighth, high IOP does NOT guarantee vision loss – many folks live with 30+ mmHg and never develop optic damage.
Ninth, lifestyle does matter: aerobic exercise can shave 1‑2 mmHg off your pressure, while excessive caffeine or smoking can push it up. Tenth, once you’ve been treated, do not think you’re done – glaucoma is chronic, and IOP can creep up again, demanding lifelong monitoring.
Bottom line: stay proactive, get regular checks, and don’t buy into the oversimplified "myths" that make you think you’re safe if you feel fine. Knowledge is your best defense against vision loss.
Landmark Apostolic Church
October 8, 2025 AT 02:06Reading through the myth‑buster, I’m reminded how often we overlook the subtle dance between physiology and daily habits. It’s fascinating that something as simple as a morning jog can gently lower IOP, while that latte you love might nudge it upward. The interplay of stress, posture, and even ambient temperature plays a role, suggesting that eye health is as much a lifestyle matter as a medical one. This perspective urges us to view our eyes not just as organs to be examined, but as partners in our everyday rhythm.
Antonio Estrada
October 8, 2025 AT 05:43I appreciate the passion, but let’s keep the conversation constructive. Both lifestyle adjustments and medical interventions have their places in a comprehensive care plan. Encouraging patients to stay active while adhering to prescribed treatments creates a balanced approach that maximizes outcomes. Collaboration between clinicians and patients is the key to sustained eye health.
Andy Jones
October 8, 2025 AT 07:56Grammar check: the article says "Goldmann remains the gold standard" – consistent usage of "gold" twice is stylistically redundant. Also, "IOP fluctuates naturally" could be tightened to "IOP naturally fluctuates." Minor edits aside, the content is solid.
Kevin Huckaby
October 8, 2025 AT 09:53Honestly, all this "myth‑busting" feels like a boring lecture – why not just tell us the juicy scandals behind pharma’s grip on eye‑drop patents? 🤔💊 The real story is how big companies push expensive meds while cheap lifestyle hacks get ignored. Wake up, folks! 👀🚀
Brandon McInnis
October 8, 2025 AT 11:16Whoa, hold on! While the drama about pharma is indeed a hot topic, let’s not forget the practical steps we can all take right now. A daily walk, balanced diet, and regular eye exams are simple actions that empower us without waiting for corporate reform. Stay hopeful and proactive!
Aaron Miller
October 8, 2025 AT 12:40Excellent point!!; however, one must also consider the geopolitical implications of medical supply chains!!!; the reliance on foreign manufacturers for essential ophthalmic drugs could jeopardize national health security!!!; therefore, domestic production must be prioritized!!!; only then can we truly safeguard our citizens' vision!!!