Statin Muscle Pain Risk Calculator
Statin Muscle Pain Risk Calculator
Based on evidence from large studies, different statins carry different risks of causing muscle pain. Select your statin to see its relative risk compared to the lowest-risk statin (fluvastatin).
Statin Comparison
Here's how all statins compare based on muscle pain risk:
- Simvastatin: Highest risk - 1.78x odds compared to pravastatin
- Atorvastatin: Moderate to high risk - 1.4x odds compared to pravastatin
- Rosuvastatin: Moderate risk - 1.2x odds compared to pravastatin
- Pravastatin: Low risk - 1.0x odds (base risk)
- Fluvastatin: Lowest risk - 0.33x odds compared to pravastatin
When you start taking a statin to lower your cholesterol, the last thing you want is to feel like your muscles are constantly sore, cramped, or weak. But if you’ve searched online for answers, you’ve probably seen alarming headlines claiming statins are to blame for widespread muscle pain. The truth? Most of that pain isn’t from the drug at all.
Statins and Muscle Pain: The Real Story
A massive 2022 study published in The Lancet looked at data from over 123,000 people taking statins versus placebo. The results were surprising: 27.1% of people on statins reported muscle pain. So did 26.6% of people on placebo. That’s a difference of just 0.5 percentage points - or 11 extra cases of muscle pain per 1,000 people in the first year. For most people, the pain isn’t caused by the statin. It’s likely coincidence, aging, overuse, or even the nocebo effect - where you expect side effects, so you feel them.
Think of it this way: if you’ve been told statins cause muscle pain, your brain starts scanning every twinge in your legs or shoulders as proof. But if you didn’t know you were taking a statin - like in a blinded trial - those same symptoms often disappear. That’s why experts say only about 1 in 15 reports of muscle pain are actually linked to the medication.
Which Statins Are Most Likely to Cause Muscle Pain?
Not all statins are the same. Their chemical structure affects how they move through your body, how strong they are, and how likely they are to cause muscle discomfort. Based on clinical data from multiple studies, here’s how the main statins rank from highest to lowest risk of muscle pain:
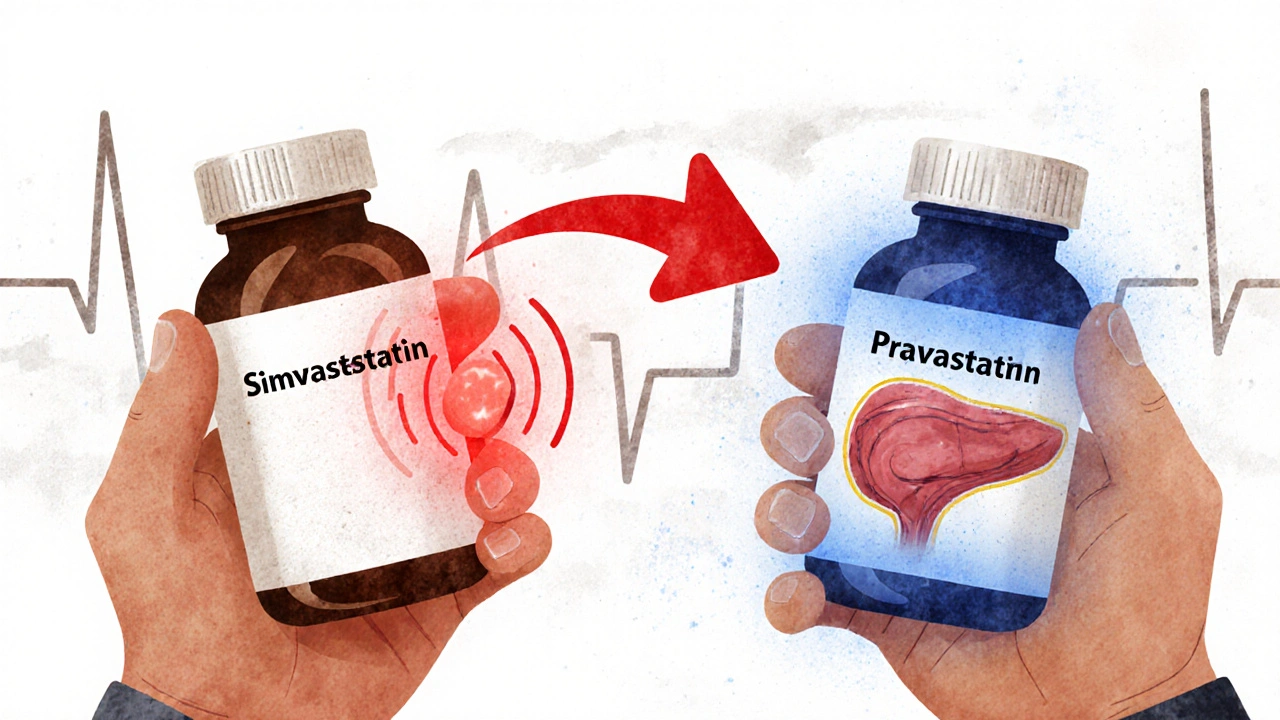
- Simvastatin - Highest risk. It’s lipophilic (fat-soluble), which lets it enter muscle tissue more easily. Studies show it has nearly twice the odds of causing muscle pain compared to pravastatin.
- Atorvastatin - Moderate to high risk. Often prescribed at higher doses, which increases side effect chances. Still, many people tolerate it fine.
- Rosuvastatin - Moderate risk. More potent than others, but less likely to enter muscle cells than simvastatin.
- Pravastatin - Low risk. Hydrophilic (water-soluble), so it stays mostly in the liver. Fewer reports of muscle issues.
- Fluvastatin - Lowest risk. Even less likely to cause muscle symptoms than pravastatin. Often overlooked but a smart choice for sensitive patients.
These rankings aren’t guesses. They’re based on odds ratios from large analyses. For example, simvastatin had an odds ratio of 1.78 compared to pravastatin - meaning you’re nearly 80% more likely to report muscle pain with simvastatin. Fluvastatin? Its odds ratio was 0.33 - meaning you’re less than one-third as likely to have muscle pain compared to pravastatin.
Why Does This Happen? The Science Behind the Pain
Statins block an enzyme called HMG-CoA reductase to lower cholesterol. But that same enzyme is also involved in making coenzyme Q10, which helps your muscles produce energy. Lower CoQ10 levels might contribute to fatigue or soreness - but studies haven’t proven this is the main cause. More importantly, muscle pain from statins usually comes with elevated creatine kinase (CK) levels - a sign of muscle damage. But in most cases, CK stays normal even when people feel pain. That’s a big clue the pain isn’t from actual muscle injury.
The real issue? Lipophilicity. Statins like simvastatin and atorvastatin dissolve easily in fat, so they slip into muscle cells. Pravastatin and fluvastatin don’t. They stay in the liver where they’re supposed to work. That’s why switching from simvastatin to pravastatin often solves the problem - not because the second drug is "milder," but because it doesn’t invade your muscles.
What Patients Are Really Experiencing
Online forums are full of stories. One person on Reddit said they stopped simvastatin after three months of leg cramps - then switched to pravastatin and had zero issues for over a year. Another did a blind test: sometimes they got the real drug, sometimes a sugar pill. Their muscle pain happened equally on both. They concluded it was all in their head - and felt relieved.
On Drugs.com, patient reviews match the science. Simvastatin has a muscle pain rating of 3.2/5. Atorvastatin is 2.9/5. Pravastatin is 2.5/5. Fluvastatin? 2.3/5. Lower scores don’t mean worse drugs - they mean fewer people report pain with them. The pattern is clear: the higher the risk profile, the more complaints.
Here’s the kicker: 78% of people who quit statins because of muscle pain never talked to their doctor. They just stopped. And most of them didn’t need to. The evidence shows that over 90% of those cases weren’t actually caused by the statin. That’s a huge missed opportunity to keep taking a life-saving medication.
What to Do If You Have Muscle Pain
If you’re on a statin and feel muscle soreness, don’t panic. Don’t quit cold turkey. Do this instead:
- Track your symptoms. When did they start? Do they happen every day? Are they worse after exercise? Write it down.
- Ask your doctor about a "statin holiday." Stop the statin for 2-4 weeks. If the pain goes away, then restart it. If it comes back, there’s a real link. If it doesn’t? The statin probably isn’t the culprit.
- Try a switch. If you’re on simvastatin or atorvastatin, ask about switching to pravastatin or fluvastatin. Many people find relief without losing cholesterol control.
- Check your dose. Sometimes lowering the dose reduces side effects. A 10 mg dose of atorvastatin may cause less pain than 40 mg - and still work well.
- Get tested for SLCO1B1 gene variant. Less than 3% of people have a genetic change that makes them more prone to statin muscle issues. If you’ve had severe pain with multiple statins, this test might help.
There’s also a proven protocol from the Mayo Clinic: educate patients about the nocebo effect, restart the statin at a very low dose, and slowly increase it over weeks. In one 2023 study, 68% of people who’d quit statins because of pain were able to get back on them using this method.
Why This Matters: The Bigger Picture
Statins prevent heart attacks and strokes. For every 100 people treated for five years, they stop about three major cardiovascular events. That’s hundreds of thousands of lives saved every year in the U.S. alone. But because of fear over muscle pain, nearly 1 in 5 new users quit within a year. That’s not just a personal loss - it’s a public health problem.
Doctors are now being trained to talk differently about statins. Instead of saying, "This might cause muscle pain," they’re saying, "Most muscle pain you feel isn’t from the statin. But let’s check to be sure." This shift is already changing how patients respond. In Europe, regulators have updated guidelines to say muscle symptoms are reported just as often with placebo as with statins.
Alternatives If You Really Can’t Tolerate Statins
If you’ve tried multiple statins and still have real muscle pain - and your doctor confirms it’s not the nocebo effect - there are other options:
- Ezetimibe - Lowers cholesterol by blocking absorption in the gut. Often used with a low-dose statin. Few side effects.
- PCSK9 inhibitors - Injectable drugs like evolocumab and alirocumab. Very effective, but expensive - around $5,850 a year. Used only when statins truly fail.
- Lifestyle changes - Diet, exercise, and weight loss can lower LDL cholesterol by 20-30% on their own. Not a replacement for medication in high-risk patients, but a powerful partner.
Don’t assume you have to live with pain. Don’t assume you have to quit. There’s a middle path - one backed by data, not fear.
Final Takeaway
Simvastatin is the statin most linked to muscle pain. Atorvastatin comes next. Pravastatin and fluvastatin are the safest bets if you’ve had issues before. But the biggest risk isn’t the drug - it’s stopping it unnecessarily. Muscle pain from statins is rare. The risk of a heart attack if you quit? That’s real. Talk to your doctor. Get tested. Try a switch. Don’t let misinformation cost you your health.
Do all statins cause muscle pain?
No. Muscle pain from statins is rare, and not all statins carry the same risk. Simvastatin and atorvastatin are more likely to cause muscle symptoms than pravastatin or fluvastatin. For most people, muscle pain is unrelated to the medication - often caused by aging, activity, or the nocebo effect.
Is muscle pain from statins dangerous?
In most cases, no. True statin-induced muscle damage (rhabdomyolysis) is extremely rare - less than 1 in 10,000 users. Most people feel soreness or fatigue without elevated creatine kinase levels, which means no actual muscle injury is happening. If you have severe pain, dark urine, or weakness, get checked immediately - but those are red flags, not common side effects.
Can I switch from simvastatin to pravastatin safely?
Yes, and many people do. Pravastatin is water-soluble and doesn’t enter muscle tissue as easily as simvastatin. Studies show it has a much lower risk of muscle pain. Your doctor can adjust the dose to match your cholesterol goals - pravastatin 40 mg is roughly equivalent to simvastatin 20 mg in effectiveness.
Why do some people say statins ruined their life?
They’re often reacting to real symptoms - but those symptoms may not be caused by the statin. The nocebo effect is powerful. If you’ve heard stories about statins causing fatigue or pain, your brain may interpret normal aches as side effects. That doesn’t make the pain fake - it just means the cause isn’t the drug. A blinded rechallenge test can help sort this out.
How do I know if my muscle pain is from a statin?
The only reliable way is through a "statin holiday" followed by re-challenge. Stop the statin for 2-4 weeks. If pain improves, restart it. If pain returns, it’s likely linked. If not, it’s probably something else. Blood tests for creatine kinase can help confirm true muscle damage, but most pain happens without elevated levels.
Kane Ren
November 22, 2025 AT 00:23Man, I was convinced my leg cramps were from simvastatin until I read this. Switched to pravastatin last month and now I’m hiking weekends like I’m 25 again. Seriously, don’t quit without trying a switch first.
Charmaine Barcelon
November 23, 2025 AT 14:12You’re all wrong. Statins are poison. I stopped mine and my energy came back. It’s not the nocebo. It’s the drugs. Period. End of story. Don’t let them trick you.
Karla Morales
November 24, 2025 AT 20:25Let’s break this down statistically. 📊 The 0.5% difference in muscle pain between statin and placebo groups? That’s statistically significant in a cohort of 123k. But clinically? Marginal. The real issue is misattribution. 🧠 People are conditioned to blame the pill. The nocebo effect is not just psychological-it’s neurobiological. Also, fluvastatin’s OR of 0.33? That’s gold. Why isn’t this first-line? 🤔
Javier Rain
November 26, 2025 AT 05:18Guys, I get it-you’re scared. I was too. But here’s the truth: statins saved my dad’s life after his stent. He was on simvastatin, hated the cramps, quit cold turkey. Two months later, he had a heart attack. We switched him to pravastatin. No pain. No issues. Don’t let fear steal your future. Talk to your doc. Try the switch. You’ve got this.
Laurie Sala
November 28, 2025 AT 00:48I’ve been on statins for 7 years… and I’ve had muscle pain EVERY SINGLE DAY… I’m not imagining it… I’m not crazy… I’m just tired… I just want to walk without my legs screaming… why won’t anyone listen… I’m not just complaining… I’m suffering…
Lisa Detanna
November 28, 2025 AT 03:58As someone raised in a culture where medicine is seen as a last resort, I used to think statins were overprescribed. But after seeing my uncle survive two heart attacks because he stayed on pravastatin, I get it. It’s not about fear. It’s about balance. The data here is clear-don’t quit without exploring options first. Your body isn’t your enemy.
Demi-Louise Brown
November 28, 2025 AT 15:04Tracking symptoms before and after a statin holiday is the most reliable method. Many patients don’t realize how much context matters. Did the pain start after a new workout routine? After a stressful month? Before or after the statin? Documenting helps separate coincidence from causation. Small steps. Big results.
Matthew Mahar
November 29, 2025 AT 11:39ok so i read this whole thing and like… i think statins are fine?? but i also think people shouldnt be scared of feeling pain?? like if your legs hurt maybe you just need to stretch?? or maybe you’re getting old?? or maybe your mattress is trash?? idk but i think we blame pills too much??
John Mackaill
December 1, 2025 AT 01:52Interesting how the UK guidelines now reflect this too. We’ve been training GPs to say, 'It's probably not the statin, but let’s check anyway.' The shift in language is subtle, but it’s working. Fewer people quit. More people stay on life-saving meds. It’s not about dismissing pain-it’s about understanding it.
Adrian Rios
December 2, 2025 AT 17:51Let me be real for a second. I used to be the guy who quit statins because of muscle pain. I thought I was being proactive. Turns out I was just scared. I didn’t know about the nocebo effect. I didn’t know simvastatin was the worst offender. I didn’t know fluvastatin existed. I didn’t know a 10mg dose of atorvastatin could work just as well as 40mg with fewer side effects. I lost a year of my life to fear. Don’t make my mistake. Talk to your doctor. Do the test. Try the switch. You’re not weak for needing help-you’re smart for seeking it.
Casper van Hoof
December 3, 2025 AT 05:54The paradox of modern pharmacology: we are simultaneously more informed and more anxious. The science is clear, yet the narrative is distorted. The body, in its infinite complexity, is reduced to a chemical ledger. Pain becomes a binary: drug or no drug. But what of the soul’s interpretation of suffering? The mind does not merely perceive-it constructs. The nocebo effect is not an error of biology, but a revelation of consciousness. Perhaps the true statin is not the pill, but the story we tell ourselves about it.
Richard Wöhrl
December 4, 2025 AT 00:27Important note: If you’re on simvastatin and have muscle pain, don’t just switch blindly. Get your CK levels checked first-even if they’re normal, it’s good baseline data. Also, check your vitamin D and thyroid levels. Low D and hypothyroidism mimic statin pain. I’ve seen 3 patients in my clinic who thought it was the statin… turned out they were vitamin D deficient. Fixed that, pain vanished. Don’t skip the basics.
Brandy Walley
December 4, 2025 AT 13:45Statins are a scam. Big Pharma made them to sell pills. Muscle pain is real. People are dying from heart disease because they’re scared to take the pills. Wait no that’s not right. Actually they’re dying because they took the pills. The system is rigged. I don’t trust doctors. I trust my body. I quit. I feel better. End of discussion.
shreyas yashas
December 5, 2025 AT 08:48in india most people dont even know what statins are. my uncle took one for 3 months then stopped because his legs hurt. he thought it was diabetes. we never told him it was the pill. he’s fine now. but he’s 70. maybe the pain was just old age. still, this post is helpful for people who actually know what’s going on.
Suresh Ramaiyan
December 6, 2025 AT 18:31There’s a quiet wisdom in this: the body speaks, but we’ve trained ourselves to hear only the loudest voice-the one that says ‘this pill is bad.’ But what if the real message is ‘listen deeper’? The pain may not be from the drug, but from the fear of the drug. And that fear? That’s something we can heal. Not with a new prescription-but with a new perspective.