When your doctor talks about switching your medication to something cheaper, you might hear the words biosimilar or generic and think they mean the same thing. They don’t. And confusing them could cost you more than just money-it could affect how well your treatment works.
Let’s cut through the noise. If you’re on a biologic for rheumatoid arthritis, Crohn’s disease, or cancer, you’ve probably seen a price tag that makes your eyes water. A single dose of Humira or Herceptin can run over $2,000. That’s why biosimilars and generics exist: to bring down costs without sacrificing safety. But they’re not interchangeable. Not even close.
What’s the Difference Between a Generic and a Biosimilar?
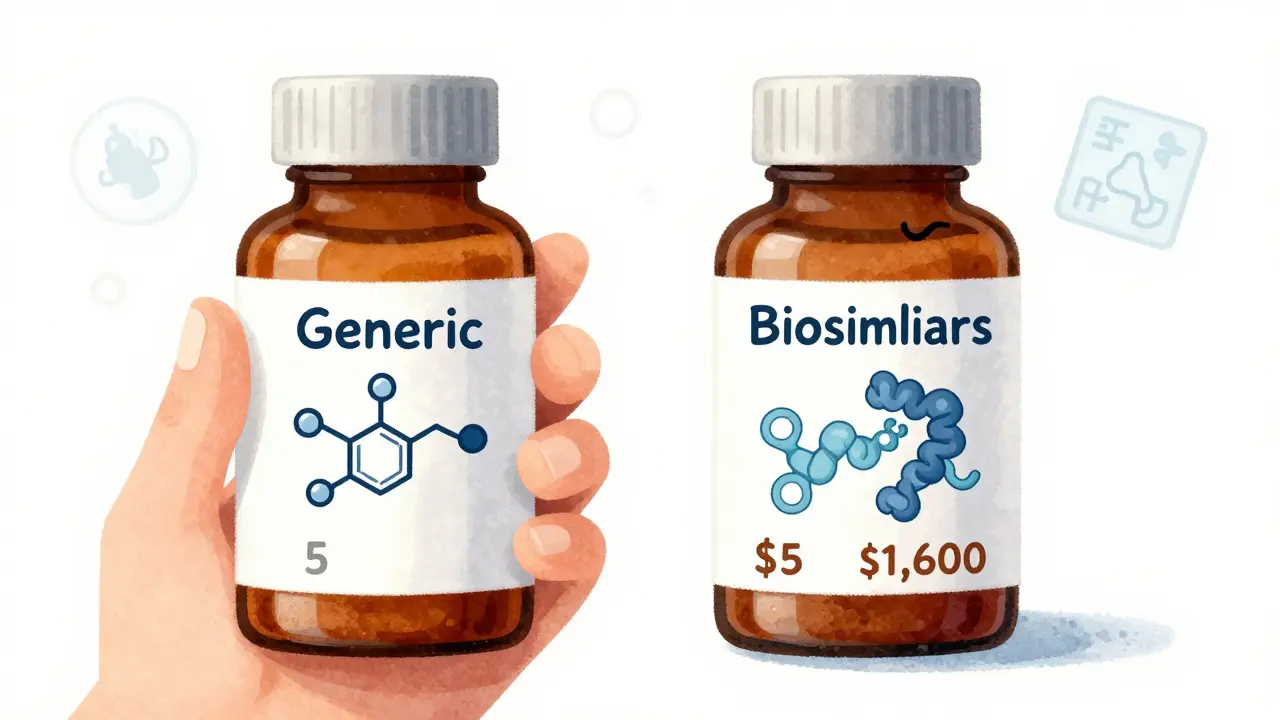
Generics are copies of small-molecule drugs-things like aspirin, metformin, or atorvastatin. They’re made in labs using chemical reactions. The molecule is simple, stable, and easy to replicate. If you take a generic version of Lipitor, you’re getting the exact same chemical structure as the brand name. The FDA requires it to be identical in active ingredient, strength, dosage form, and how your body absorbs it.
Biosimilars are different. They’re copies of biologics-medicines made from living cells. Think insulin, antibodies like adalimumab, or cancer drugs like trastuzumab. These aren’t just molecules. They’re complex, three-dimensional proteins that fold in precise ways to work correctly. Even tiny changes in the manufacturing process-like using a different type of hamster cell to grow them-can alter their shape slightly. That’s why biosimilars aren’t exact copies. They’re “highly similar.”
The FDA says biosimilars must show no “clinically meaningful differences” in safety, purity, or potency compared to the original. That sounds reassuring, but it’s not the same as being identical. Generics are. Biosimilars are close.
Cost Savings: How Much Do You Really Save?
Generics save you a lot. On average, they cost 80-85% less than the brand-name drug. A 30-day supply of generic lisinopril might be $5. The brand? $150. That’s a no-brainer.
Biosimilars? Not so dramatic. They typically save you 15-20% off the original biologic price. That still adds up-especially if you’re getting infusions every few weeks. But it’s not a 90% drop. Why? Because making a biosimilar isn’t cheap. It costs $100-250 million and takes 8-10 years to develop. Generics? Around $2-3 million and 3-4 years.
So if you’re choosing between a generic and a biosimilar, you’re not comparing apples to apples. You’re comparing a $5 pill to a $1,600 injection. The biosimilar saves you $300-$400 a month. The generic saves you $145. Both are good. But they’re used in totally different situations.
When Can You Switch? And Who Decides?
With generics, switching is easy. In 49 U.S. states, your pharmacist can swap your brand-name drug for a generic without asking your doctor-unless the doctor wrote “dispense as written.” You probably didn’t even notice when your pill changed color or shape.
Biosimilars? Not so simple. Only those labeled “interchangeable” can be swapped at the pharmacy without your doctor’s permission. And even then, 28 states require the pharmacist to notify your doctor within 72 hours. Why? Because biologics are tricky. If you switch back and forth between a reference product and a biosimilar, could your immune system react? It’s rare-but it’s why regulators are cautious.
Right now, only a handful of biosimilars have received interchangeable status. The first was Semglee (insulin glargine) in 2021. Then Cyltezo (adalimumab) in 2023. More are coming. But most biosimilars still require your doctor to specifically prescribe them.

Real-World Experience: What Do Patients Actually Say?
People who’ve switched to biosimilars report mixed feelings. One rheumatoid arthritis patient on PatientsLikeMe said: “I saved $8,000 a year. My symptoms didn’t change. My doctor explained the science, and that made me feel safe.”
But another survey from the National Psoriasis Foundation found 42% of patients were worried biosimilars wouldn’t work as well. Some people just feel more comfortable with the drug they’ve been on for years-even if it’s more expensive.
And then there are the little things. One Reddit user, a pharmacist, shared that elderly patients struggled with the different pen design on Basaglar (a biosimilar insulin). The original Lantus pen had a click you felt. Basaglar’s click was softer. Some patients missed their dose because they didn’t hear or feel it.
In cancer care, the story’s different. A colon cancer patient wrote: “My out-of-pocket dropped from $450 to $75 per infusion. My tumor markers stayed stable. No side effects.”
Studies back this up. A 2022 review of 128 studies involving over 38,000 patients found no difference in safety or effectiveness between reference infliximab and its biosimilar. The FDA’s adverse event database shows biosimilars have nearly identical safety profiles.
But anxiety isn’t just in your head. If you’re scared, your body reacts. That’s why education matters more than you think.
What Your Doctor Needs to Know
Not all doctors are up to speed. A 2023 AMA survey found only 58% of non-specialist physicians felt very confident prescribing biosimilars. Compare that to 89% who felt confident with generics.
Why? Because biosimilars come with extra layers. You need to know about:
- Interchangeability status
- State substitution laws
- Prior authorization hurdles
- Manufacturer support programs
Many biosimilar makers-like Amgen or Sandoz-offer support programs that help with paperwork, copay assistance, and even nurse education for patients. Generics? No one calls you. You just pick up your prescription.
If your doctor isn’t familiar with biosimilars, ask for a referral to a specialist or a pharmacy team. You deserve to understand your options.
Storage, Handling, and Logistics
Generics? Most sit on your shelf at room temperature. You can leave them in your car for a few hours. No problem.
Biosimilars? They’re fragile. Most need to be kept between 2°C and 8°C-like a fridge. If they get too warm, the protein can unfold and stop working. Some even need protection from light.
This affects pharmacies, home delivery services, and even how you store your medication at home. If you’re traveling, you need a cooler. If you’re on Medicare, your infusion center handles it. But if you’re self-injecting, you’re responsible.
What Should You Do?
Here’s a simple decision tree:
- Is your drug a small molecule? (e.g., blood pressure pill, thyroid med, statin) → Go for the generic. It’s safe, cheap, and proven.
- Is your drug a biologic? (e.g., Humira, Enbrel, Herceptin, Rituxan) → Ask about biosimilars. They’re not perfect copies, but they’re safe and can cut your costs significantly.
- Are you nervous about switching? Talk to your doctor. Ask for data. Ask if the biosimilar is interchangeable. Ask if there’s a support program.
- Are you on a tight budget? Even a 20% savings on a $2,000 drug is $400 a month. That’s a rent payment.
Don’t let fear stop you. The science is solid. The FDA approves biosimilars with the same rigor as the original. Real-world data backs it up. The only thing holding people back is misinformation.
What’s Next?
The next big wave is coming. In 2024, biosimilars for Stelara (ustekinumab) are expected to hit the market. That’s a $5 billion-a-year drug. When it happens, prices could drop even more.
The Inflation Reduction Act of 2022 removed financial penalties for doctors who use biosimilars in Medicare. That’s already pushing more providers to prescribe them.
By 2027, experts predict biosimilars will make up 45% of all biologic prescriptions-up from 22% today.
Change is coming. And it’s not just about money. It’s about access. More people will get life-saving treatments because biosimilars make them affordable.
Know your options. Ask questions. Don’t assume. And don’t let a label scare you. Your health matters. So does your wallet. You don’t have to choose one over the other.
Kelly Weinhold
January 31, 2026 AT 17:54Okay but can we talk about how wild it is that we’re still arguing over whether a biosimilar is ‘good enough’ when the data says it’s basically the same? I’ve been on a biosimilar for RA for three years now-same energy, same joint pain relief, same zero drama. My wallet thanks me, my body doesn’t care, and my doctor high-fives me every time the pharmacy refills it. Why are we still treating this like a scary leap when it’s basically just a cheaper version of the same thing? The fear is real, but the science? Solid. Stop overthinking it.
Sheila Garfield
February 1, 2026 AT 14:11I get why people are nervous-my mum switched to a biosimilar insulin and kept saying she ‘felt’ it wasn’t working, even though her HbA1c was identical. Turns out she missed the click on the pen. That’s the real issue, not the drug. It’s not about efficacy, it’s about trust, routine, and the little things that make us feel safe. Maybe we need better patient education, not just more biosimilars.
Shawn Peck
February 2, 2026 AT 06:27Y’all are overcomplicating this. Generic = same chemical. Biosimilar = close enough. If your insurance pushes it, take it. If you panic, don’t. It’s not magic. It’s science. Stop listening to Reddit memes and read the FDA’s actual data. I’ve seen people lose their minds over a $300 savings like it’s a betrayal. Chill. Your body doesn’t know the brand name.
Niamh Trihy
February 3, 2026 AT 17:12One thing nobody talks about: biosimilars often come with better patient support programs. I got free training, a nurse hotline, and even a cooler for travel with my biosimilar insulin. The generic I took for blood pressure? No one called. Just a pill in a bottle. So yeah, the drug’s cheaper-but the support might be better. That’s worth something.
Sarah Blevins
February 5, 2026 AT 06:56While the data supports biosimilar equivalence, the regulatory framework remains inconsistent across jurisdictions. The lack of harmonized substitution laws introduces clinical uncertainty, particularly in polypharmacy populations. Furthermore, pharmacovigilance systems are not adequately equipped to isolate adverse events attributable to biosimilars versus originators, creating a surveillance gap.
Jason Xin
February 7, 2026 AT 02:47Wow. So we’ve turned saving $400 a month into a philosophical debate about protein folding. I get it-change is scary. But if your tumor markers are stable and your bank account isn’t crying, maybe stop treating your meds like a sacred relic. Also, the fact that people are still worried about pen clicks? That’s the real tragedy here.
Gaurav Meena
February 8, 2026 AT 14:03Hey everyone! Just wanted to say big UP to the folks who are pushing biosimilars forward! 🙌 I’m from India, and here, access to biologics is almost impossible unless you’re rich. Biosimilars? They’ve saved lives. My cousin with Crohn’s switched and now she can work again. Yes, the science is complex-but the impact? Simple. More people treated. Less suffering. Let’s not let fear block progress. We got this! 💪❤️
kate jones
February 9, 2026 AT 15:43The distinction between interchangeability and biosimilarity is often conflated in public discourse, resulting in suboptimal therapeutic decision-making. The FDA’s criteria for interchangeability require additional analytical, pharmacokinetic, and immunogenicity studies beyond those required for biosimilarity. This regulatory tiering is critical for ensuring clinical continuity in chronic disease management, particularly in autoimmune conditions where immune sensitization may occur with multiple product switches.
Natasha Plebani
February 10, 2026 AT 02:32It’s fascinating how we treat molecules like they have souls. We give brand-name drugs dignity, rituals, even names-Humira, Herceptin-like they’re characters in a story. But when you strip away the branding, the science says they’re just proteins doing their job. The fear isn’t about the drug. It’s about losing control. About not knowing if you’re getting the ‘real’ thing. But what’s real? The label? Or the outcome? Maybe the question isn’t whether biosimilars work-it’s whether we’re ready to stop assigning meaning to packaging.
Kimberly Reker
February 10, 2026 AT 08:03My mom’s on a biosimilar for MS. She was scared. So I made her a little chart: old drug cost = $2,100/month. New drug cost = $1,700/month. Same side effects. Same results. She looked at it, shrugged, and said, ‘Well, I guess my body doesn’t care about the logo.’ She’s been fine for 18 months. Sometimes the best medicine is just a quiet conversation and a spreadsheet.