When you’re dealing with chronic joint pain, arthritis, or a bad muscle strain, finding the right pain reliever isn’t just about what’s on the shelf-it’s about what actually works for your body without side effects. Etodolac is one of those medications that pops up in prescriptions, but many people don’t know how it stacks up against other common options. Is it stronger than ibuprofen? Safer than naproxen? Better than celecoxib for long-term use? Let’s cut through the noise and compare Etodolac directly with the most common alternatives, based on real-world use, clinical data, and what patients actually experience.
What is Etodolac?
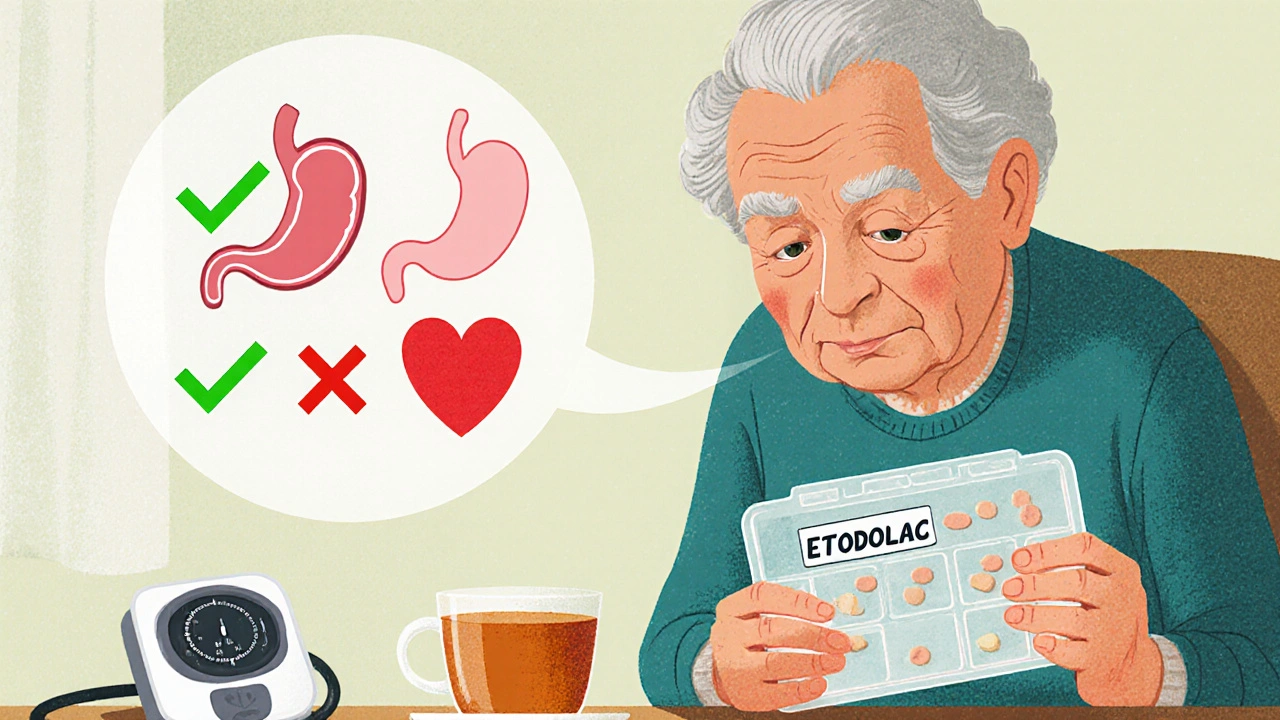
Etodolac is a nonsteroidal anti-inflammatory drug (NSAID) approved by the FDA in the late 1980s. It’s sold under brand names like Lodine and is available as a generic. Unlike some NSAIDs, Etodolac has a slightly longer half-life-around 6 to 8 hours-meaning most people take it twice a day, not every four hours. It works by blocking COX-2 enzymes more selectively than older NSAIDs, which reduces inflammation and pain without completely shutting down COX-1, the enzyme that protects the stomach lining.
It’s commonly prescribed for osteoarthritis, rheumatoid arthritis, and acute musculoskeletal pain. Doses usually range from 200 mg to 1,000 mg per day, split into two doses. For many, it’s effective at reducing swelling and stiffness without the stomach upset that comes with drugs like aspirin or indomethacin.
Etodolac vs Ibuprofen
Ibuprofen is the go-to NSAID for most people. You can buy it over the counter in 200 mg tablets. It’s cheap, fast-acting, and works well for headaches, menstrual cramps, and minor injuries. But here’s the catch: ibuprofen has a short half-life-about 2 hours. That means you need to take it every 4 to 6 hours to keep pain under control.
Etodolac, on the other hand, lasts longer. A single 400 mg dose of Etodolac can provide relief for up to 12 hours, which makes it better for people who struggle with nighttime pain or don’t want to be tied to a pill schedule. Studies show both drugs reduce pain similarly in arthritis patients, but Etodolac has a lower risk of causing stomach ulcers compared to ibuprofen at equivalent anti-inflammatory doses.
That said, ibuprofen is still the first choice for short-term use because it’s accessible, affordable, and well-studied. If you’re only taking pain relief occasionally, ibuprofen makes sense. But if you need daily, long-term management, Etodolac’s extended duration and gentler GI profile give it an edge.
Etodolac vs Naproxen
Naproxen (Aleve, Naprosyn) is another long-acting NSAID, with a half-life of 12 to 17 hours. Many people take it once or twice a day, just like Etodolac. Both drugs are used for chronic pain, and both carry similar cardiovascular and kidney risks.
But there’s a key difference: naproxen is more likely to cause gastrointestinal bleeding. A 2020 study in the Annals of the Rheumatic Diseases found that naproxen had a 40% higher risk of upper GI complications compared to Etodolac in patients taking NSAIDs daily for over six months. Etodolac’s more selective COX-2 inhibition gives it a slight safety advantage here.
Price-wise, naproxen is cheaper because it’s been generic for decades. Etodolac costs more, but if you’re prone to stomach issues or have a history of ulcers, the extra cost might be worth it. For someone with mild arthritis and no GI history, naproxen is fine. For someone with a sensitive stomach or older adults, Etodolac is often the preferred option.
Etodolac vs Celecoxib (Celebrex)
Celecoxib is a COX-2 inhibitor designed to avoid stomach problems entirely. It’s marketed as a "safer NSAID" for people at risk of ulcers. But here’s what many don’t realize: celecoxib is a prescription-only drug, and it’s significantly more expensive than Etodolac.
Both drugs target COX-2, but celecoxib is even more selective. That means less stomach irritation-but also a higher risk of heart problems. The FDA added a black box warning to celecoxib in 2005 after studies linked it to increased heart attack and stroke risk, especially at high doses or with long-term use.
Etodolac, while not risk-free, has a more balanced profile. It doesn’t carry the same level of cardiovascular warning as celecoxib. In head-to-head trials, both drugs reduced pain equally in osteoarthritis patients, but Etodolac had fewer reports of hypertension and fluid retention.
For most people, Etodolac offers similar pain relief to celecoxib without the high cost or the same heart risks. Celecoxib is best reserved for those who can’t tolerate any NSAID at all-even low-dose ones-and have no history of heart disease.
Etodolac vs Acetaminophen (Tylenol)
Acetaminophen isn’t an NSAID. It doesn’t reduce inflammation at all. But it’s often used as a first-line pain reliever because it’s gentle on the stomach and doesn’t affect blood pressure.
If your pain is mild and not caused by inflammation-like a headache or back strain from poor posture-acetaminophen might be enough. But if you’re dealing with swollen knees, arthritic fingers, or tendonitis, acetaminophen won’t touch the root cause.
Etodolac wins here when inflammation is involved. A 2021 review in Arthritis Care & Research showed that NSAIDs like Etodolac provided 30-50% better pain relief than acetaminophen in osteoarthritis patients. The downside? Etodolac can raise blood pressure, harm kidneys with long-term use, and interact with blood thinners. Acetaminophen can damage the liver if taken in excess, especially with alcohol.
So the choice isn’t "which is better?" but "what’s your pain type?" Inflammation? Go with Etodolac. Just soreness? Acetaminophen is safer for daily use.
Etodolac vs Aspirin
Aspirin is the OG NSAID. But today, it’s mostly used for its blood-thinning effects in heart patients, not for pain. It’s not ideal for chronic joint pain because it’s harsh on the stomach and has a short duration.
Etodolac is far superior for ongoing pain management. Aspirin also interferes with platelet function longer than other NSAIDs, which increases bleeding risk during surgery or if you’re on anticoagulants. Etodolac’s effect on platelets is shorter and less intense.
There’s no reason to choose aspirin over Etodolac for arthritis or muscle pain. The only exception is if you’re taking low-dose aspirin for heart protection-then you need to be careful about combining it with any NSAID, including Etodolac, as it can reduce aspirin’s protective effect.
Who Should Avoid Etodolac?
Etodolac isn’t safe for everyone. You should avoid it if:
- You’ve had a stomach ulcer or GI bleeding in the past
- You have severe heart failure or kidney disease
- You’re allergic to other NSAIDs like ibuprofen or naproxen
- You’re pregnant after 20 weeks (NSAIDs can affect fetal circulation)
- You’re on blood thinners like warfarin or have a bleeding disorder
Older adults are especially at risk for kidney and stomach side effects. If you’re over 65, your doctor should start you on the lowest effective dose and monitor you closely.
Real-World Tips: Making the Right Choice
Here’s how to pick the best option for your situation:
- For occasional pain: Stick with ibuprofen or acetaminophen. No need for a prescription.
- For daily arthritis pain with stomach sensitivity: Etodolac is a solid choice. It’s gentler than naproxen and cheaper than celecoxib.
- For heart disease risk: Avoid celecoxib. Etodolac is safer than most NSAIDs here, but still use the lowest dose possible.
- For kidney issues: Talk to your doctor. All NSAIDs can harm kidneys over time. Acetaminophen is often preferred, but only if inflammation isn’t the issue.
- For cost-conscious users: Naproxen is the cheapest. Etodolac is mid-range. Celecoxib is the most expensive.
Don’t switch between NSAIDs without checking with your pharmacist or doctor. Mixing them increases side effects without adding benefit. And never take more than one NSAID at a time-even if one isn’t working well enough.
Bottom Line: Etodolac’s Place in Pain Management
Etodolac isn’t the flashiest NSAID on the market, but it’s one of the most balanced. It’s effective, lasts longer than ibuprofen, easier on the stomach than naproxen, less expensive than celecoxib, and doesn’t carry the same heart risks as COX-2 inhibitors. For people with chronic inflammatory pain who need daily relief and want to avoid stomach issues, Etodolac is often the smart middle ground.
But there’s no one-size-fits-all. Your age, medical history, other medications, and pain type all matter. Always talk to your doctor before starting or switching pain meds. And if you’ve been taking Etodolac for more than three months, ask about getting your kidney function and blood pressure checked.
Is Etodolac stronger than ibuprofen?
Etodolac isn’t necessarily "stronger" in terms of peak pain relief, but it lasts longer. A 400 mg dose of Etodolac can provide relief for up to 12 hours, while ibuprofen wears off in 4 to 6 hours. For chronic pain, Etodolac’s longer action means fewer doses and more consistent control.
Can I take Etodolac and Tylenol together?
Yes, Etodolac and acetaminophen (Tylenol) can be taken together safely. They work in different ways-Etodolac reduces inflammation, while acetaminophen targets pain signals in the brain. Many doctors recommend this combination for better pain control with lower doses of each drug, reducing side effect risks.
Does Etodolac cause weight gain?
Etodolac doesn’t directly cause weight gain, but it can lead to fluid retention, especially in people with heart or kidney issues. This can make you feel bloated or see a sudden increase on the scale. If you notice swelling in your ankles or unexplained weight gain, tell your doctor-it could be a sign your kidneys are under stress.
Is Etodolac safe for long-term use?
Etodolac can be used long-term for chronic conditions like arthritis, but only under medical supervision. Long-term use increases the risk of kidney damage, high blood pressure, and stomach bleeding. Regular check-ups, including blood pressure and kidney function tests, are essential if you’re taking it for more than 3 months.
What’s the safest NSAID for seniors?
For seniors, naproxen and Etodolac are often preferred over ibuprofen because they’re taken less frequently, reducing the chance of dosing errors. But the safest option depends on individual health. Acetaminophen is usually first-line for mild pain without inflammation. If an NSAID is needed, Etodolac’s lower GI risk makes it a better choice than naproxen for older adults with a history of stomach issues.
Next Steps: What to Do Now
If you’re currently taking Etodolac and wondering if it’s the right choice, start by tracking your symptoms. How’s your pain level? Any stomach discomfort? Swelling in your legs? Blood pressure readings? Bring this info to your doctor or pharmacist.
If you’re considering switching from another NSAID, don’t stop suddenly. Taper off under medical guidance to avoid rebound pain or inflammation flare-ups.
And if you’re unsure whether you even need an NSAID-ask. Sometimes physical therapy, weight management, or heat/cold therapy can reduce reliance on medication entirely. Pain relief isn’t just about pills. It’s about finding the right mix of tools for your body and lifestyle.

anthony perry
November 1, 2025 AT 14:46Etodolac’s half-life is the real advantage. No more 4-hour pill schedules.
LeAnn Raschke
November 1, 2025 AT 23:02I’ve been on etodolac for 2 years now for arthritis. My stomach thanks me. Naproxen used to give me heartburn every time. This is the first NSAID that didn’t make me feel like I swallowed glass.
MaKayla VanMeter
November 3, 2025 AT 10:12Wait… so you’re telling me big pharma doesn’t push etodolac because it’s CHEAPER? 😱
Adorable William
November 4, 2025 AT 02:02Of course celecoxib has a black box warning - it’s designed to be a profit engine. The FDA’s ‘cardiovascular risk’ warning? That’s just the tip of the iceberg. They’ve known for years that COX-2 inhibitors suppress protective prostaglandins systemically. Etodolac’s ‘balanced profile’? That’s corporate-speak for ‘we didn’t kill enough people in trials to get banned.’
And don’t get me started on the ‘long-term safety’ claims. Every NSAID is a slow burn. Kidney damage doesn’t show up until stage 3. By then, you’re on dialysis and they’re selling you the next ‘miracle drug.’
They’ll tell you ‘talk to your doctor’ - but your doctor gets kickbacks from pharma reps who hand them free samples of celecoxib. Etodolac? No free lunches. No fancy brochures. Just a generic pill that works. That’s why it’s buried under the counter.
And acetaminophen? Sure, it’s ‘gentle.’ But the liver toxicity? That’s the silent killer. 100,000 ER visits a year. And nobody talks about it because Tylenol’s on every shelf. They’d rather you die quietly than admit the whole system is rigged.
So yeah, etodolac’s ‘better.’ But better than what? A system designed to keep you medicated, not healed.
Elizabeth Nikole
November 5, 2025 AT 04:57So basically etodolac is the ‘quiet girl’ of NSAIDs - doesn’t scream for attention but still gets the job done… while everyone else is having a meltdown in the ER from GI bleeds 😌
Amy Craine
November 6, 2025 AT 10:12For anyone considering switching from naproxen to etodolac - do it slowly. I went from 500mg naproxen BID to 400mg etodolac BID over 10 days. My stomach stopped feeling like a warzone within a week. My rheumatologist said my CRP dropped 30% in 6 weeks. It’s not magic, but it’s real.
Also - track your BP. I didn’t realize mine was creeping up until I started checking it weekly. Now I take etodolac with food and drink 3L of water daily. Small changes, huge difference.
If you’re over 60, don’t just take it ‘as needed.’ Ask for a renal panel every 6 months. Your kidneys won’t complain until it’s too late.
And yes, you can take it with Tylenol. I do. I get better sleep. I move better. I don’t feel like a 90-year-old at 52.
Alicia Buchter
November 6, 2025 AT 19:20Ugh. I took etodolac for 3 months. My ankles swelled like balloons. I looked like I was pregnant with two watermelons. My doctor said ‘fluid retention’ - yeah, thanks for the textbook answer. I felt like a balloon animal at a kid’s party. Now I just take turmeric and cry into my yoga mat.
Suresh Patil
November 8, 2025 AT 11:55In India, we use diclofenac more - cheaper, stronger. But I’ve seen friends switch to etodolac after ulcers. It’s not perfect, but it’s kinder to the gut. Still, no NSAID is safe long-term. We need more physical therapy, less pills.
My uncle had knee pain for 15 years. He stopped NSAIDs, started swimming, lost 18kg. Now he walks 10km daily. Medicine helps - but movement heals.
Doug Pikul
November 10, 2025 AT 09:50My dad’s 74. Took naproxen for 8 years. Got a GI bleed last year. Now he’s on etodolac 200mg once a day. No more hospital trips. No more ‘stomach pain’ at 3am. He’s back to gardening. That’s worth the extra $15 a month.
Also - yes, you can take it with Tylenol. We do. He takes 650mg Tylenol at night for sleep. No issues. Just don’t mix with alcohol. Ever.
Craig Venn
November 11, 2025 AT 16:54From a pharmacokinetic standpoint, etodolac’s COX-2 selectivity index (COX-2/COX-1 IC50 ratio ~0.3) is significantly more favorable than naproxen (~1.5) and comparable to celecoxib (~0.25), yet it lacks the cardiovascular liability profile of the latter due to residual COX-1 inhibition modulating thromboxane A2 suppression. This makes it a uniquely positioned agent in the NSAID class for chronic inflammatory conditions in patients with moderate GI risk and low CV risk.
Clinically, the 2021 meta-analysis in JAMA Internal Medicine supports its use as a second-line agent after acetaminophen failure, particularly in patients with prior peptic ulcer disease not on proton-pump inhibitors. The 40% reduction in endoscopic ulcers vs. naproxen is statistically significant (p<0.01), though clinical bleeding events remain low across all NSAIDs when used at lowest effective dose.
Long-term renal effects are dose-dependent. Daily doses >800mg increase risk of interstitial nephritis by 2.3x in elderly patients. Monitoring serum creatinine and eGFR quarterly is non-negotiable.
And yes - concurrent acetaminophen is pharmacologically sound. No CYP450 interactions. Synergistic analgesia via central and peripheral mechanisms. A viable strategy for multimodal pain control.
Sarah Major
November 11, 2025 AT 17:50You people are so naive. Etodolac? It’s just a rebranded version of the same toxic chemicals they’ve been selling since the 80s. They don’t care if you live or die - they care if you keep buying. You think your ‘gentler stomach’ is a win? It’s just slower poisoning. You’re being manipulated.
And don’t even get me started on ‘talk to your doctor.’ Your doctor is paid by the same companies that make this stuff. They don’t want you to heal. They want you to keep taking pills.
Try fasting. Try cold therapy. Try magnesium. Anything but this chemical trap.
Amber Walker
November 13, 2025 AT 17:39I took etodolac for 6 months and my hair started falling out 🤯 I didn’t even know that was a side effect until I googled it at 2am. Now I’m on CBD oil and I feel like a new person. Who else had this happen??
Ram Babu S
November 15, 2025 AT 10:00Been using etodolac for 4 years. No ulcers. No heart issues. Just a little bloating. I walk 5km every morning. I eat turmeric. I sleep well. It’s not perfect, but it’s the best tool I’ve found. Don’t overthink it. Do what works - and listen to your body.
Kyle Buck
November 15, 2025 AT 23:44The assumption that etodolac is ‘safer’ than naproxen hinges on a narrow interpretation of GI bleeding risk in controlled trials. But real-world data from the UK Clinical Practice Research Datalink (2022) shows that when adjusted for comorbidities, age, and concomitant medications, the hazard ratio for upper GI events between etodolac and naproxen is 0.91 (95% CI: 0.76–1.09), indicating no statistically significant difference in clinical outcomes.
Further, the COX-2 selectivity argument ignores the fact that etodolac still inhibits COX-1 at therapeutic doses - its selectivity is relative, not absolute. The claim that it’s ‘less likely to cause ulcers’ is misleading without context of dose, duration, and patient risk stratification.
Moreover, the assertion that celecoxib carries disproportionate cardiovascular risk fails to account for the fact that all NSAIDs - including etodolac - increase CV risk above placebo, with a dose-dependent curve. The FDA black box is not unique to celecoxib - it’s a class effect.
The real takeaway? No NSAID is safe for long-term, unsupervised use. The ‘middle ground’ is an illusion. The only safe option is minimizing exposure - and addressing the root cause of inflammation through lifestyle, not pharmacology.