Fentanyl Patch Heat Exposure Risk Calculator
Fentanyl patches are designed for controlled absorption over 72 hours. Heat exposure can significantly increase absorption rates, leading to overdose risk. This calculator helps you understand your current risk based on heat exposure and other factors.
When you're managing chronic pain with a fentanyl patch, the last thing you expect is for something as simple as a hot shower or a heating pad to put your life at risk. But that’s exactly what can happen. Fentanyl patches are designed to release a steady, controlled dose of opioid painkiller through your skin over three days. But when heat is involved, that control vanishes - and the amount of fentanyl flooding into your bloodstream can jump by more than 30%. That’s not a small increase. It’s the difference between relief and respiratory failure.
How Fentanyl Patches Are Supposed to Work
Fentanyl patches, like Duragesic, are made to deliver a slow, steady stream of the drug. They’re not like pills you swallow and feel right away. Instead, the fentanyl sits in a gel layer under the patch, and over 24 to 72 hours, it slowly moves through your skin into your bloodstream. Peak levels don’t hit until about 12 to 24 hours after you apply it. That’s why doctors only prescribe them to people who are already used to opioids - someone who’s never taken strong painkillers could overdose from just one patch.The patch’s design is precise. It relies on your skin’s natural barrier to control how fast the drug gets absorbed. But that barrier isn’t foolproof. Heat changes everything.
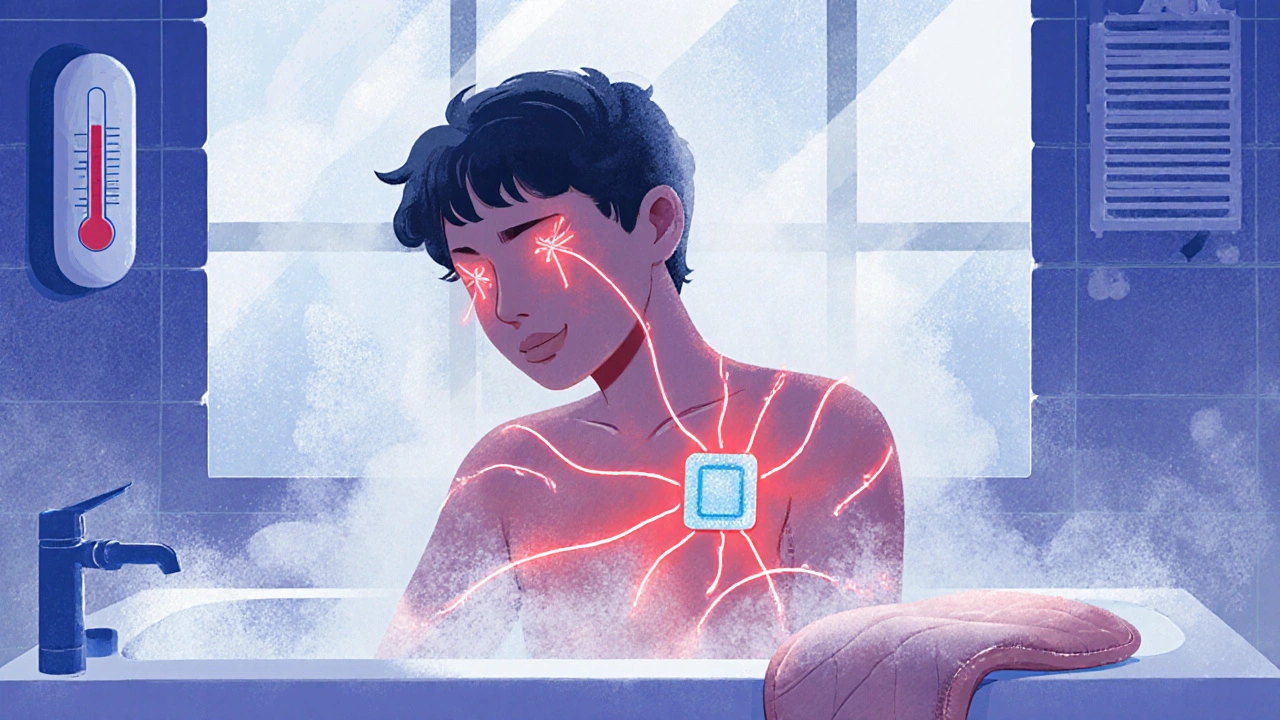
Why Heat Makes Fentanyl Patches Dangerous
Your skin has tiny blood vessels just beneath the surface. When your body temperature rises, those vessels widen. Blood flows faster. And that means more fentanyl gets pulled into your system - way faster than the patch was meant to release it.Studies show that when skin temperature hits 40°C (104°F), fentanyl levels in the blood can spike by 33%. In one controlled experiment, researchers placed a special heating patch over a fentanyl patch. Within four hours, blood levels of fentanyl tripled. That’s not theoretical. Real patients have died from this.
Three documented cases from the Medical Letter involved patients who:
- Used a heating pad for back pain
- Were wrapped in a warming blanket during surgery
- Did intense physical activity that raised their core temperature
All three developed severe respiratory depression - their breathing slowed to dangerous levels - and needed emergency treatment. One didn’t survive.
Heat Sources You Might Not Realize Are Risky
It’s not just heating pads and hot tubs. Many everyday things can raise your skin or body temperature enough to cause trouble:- Electric blankets
- Saunas and steam rooms
- Hot baths or long showers
- Sunbathing or tanning lamps
- Heated car seats
- Fever from infection
- Strenuous exercise
- Hot weather or humid environments
Even something as simple as lying on a warm radiator or sitting near a space heater can be risky. The Mayo Clinic explicitly warns patients to avoid all of these. And if you develop a fever - even a mild one - you should call your doctor immediately. Your body is already working harder to fight infection. Adding extra fentanyl on top of that can be deadly.
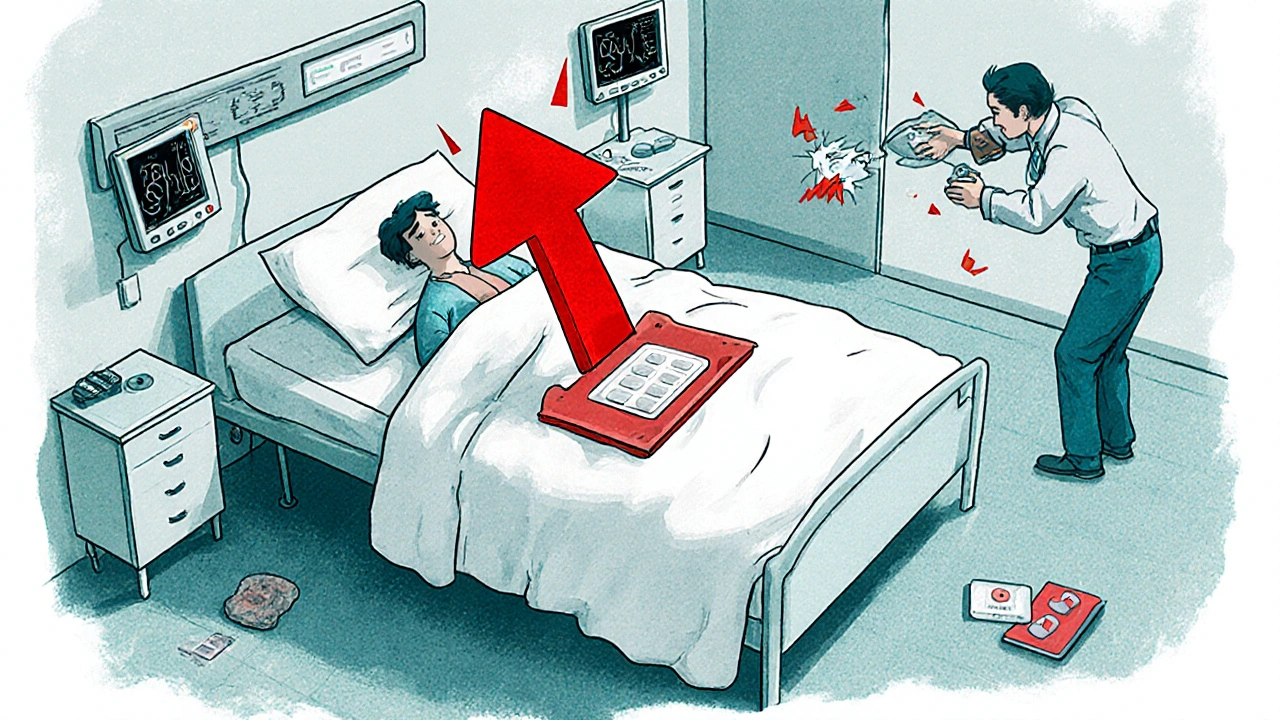
What Happens After You Remove the Patch?
A lot of people think the danger ends when they peel off the patch. It doesn’t. Even after removal, the fentanyl still trapped in your skin keeps being absorbed for several hours - sometimes up to 24 hours. That means if you take a hot shower right after removing the patch, or wrap yourself in a blanket because you’re chilly, you’re still at risk.That’s why doctors tell patients to fold the used patch in half with the sticky sides together and throw it away where kids or pets can’t reach it. The patch still contains enough drug to kill someone else.
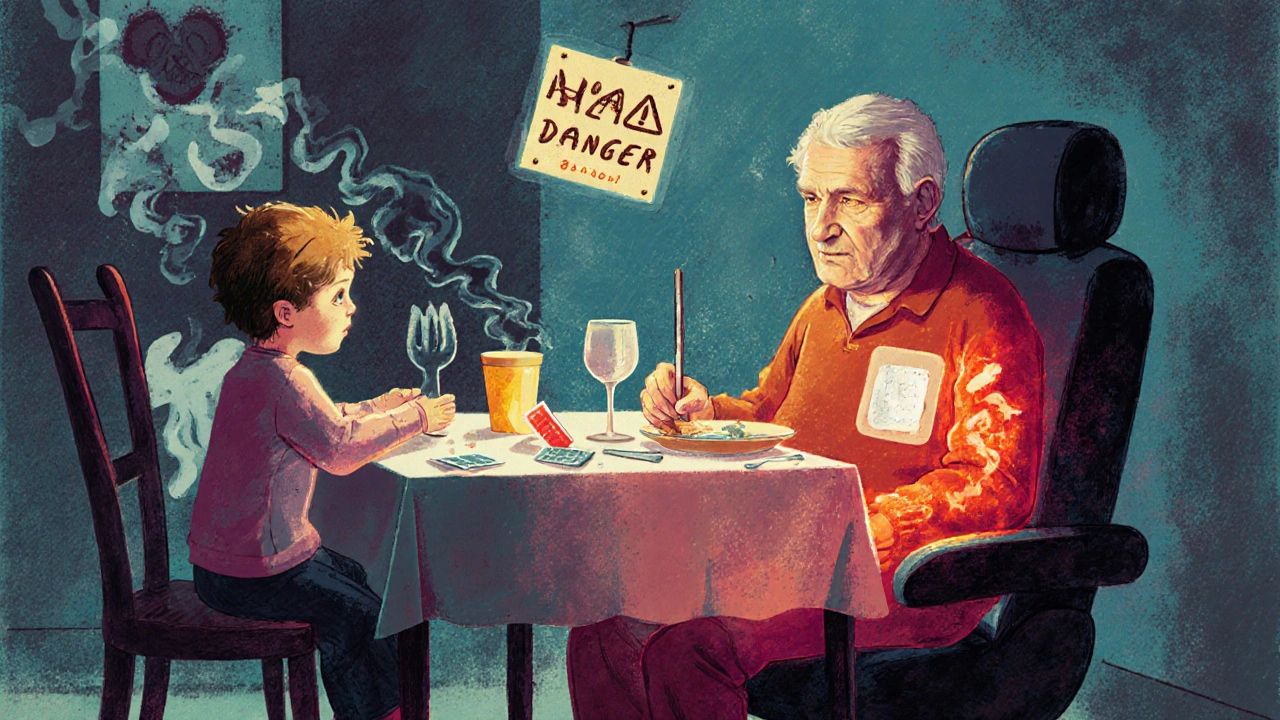
Other Drugs Can Make It Worse
Fentanyl is broken down in your liver by an enzyme called CYP3A4. If you’re taking anything that blocks this enzyme, your body can’t clear the drug fast enough. That means even normal patch doses can build up to toxic levels.Common medications that interfere with CYP3A4 include:
- Ketoconazole (an antifungal)
- Erythromycin (an antibiotic)
- Clarithromycin (another antibiotic)
- Some HIV medications
- Some antidepressants
If you’re on any of these, your doctor needs to know you’re using a fentanyl patch. A simple drug interaction can turn a safe treatment into a life-threatening one.
Warning Signs You’re Overdosing
You don’t have to wait until you’re unconscious to realize something’s wrong. Early signs of fentanyl overdose include:- Extreme drowsiness or confusion
- Slow, shallow, or irregular breathing
- Dizziness or fainting
- Pinpoint pupils
- Cold, clammy skin
- Blue lips or fingernails
Some people also develop opioid-induced hyperalgesia - where the pain gets worse instead of better - or serotonin syndrome, which includes:
- High fever
- Fast heart rate
- Muscle stiffness or spasms
- Agitation or hallucinations
If you notice any of these, remove the patch immediately and get help. Don’t wait. Fentanyl overdoses can kill in minutes.
Who Shouldn’t Use Fentanyl Patches at All
Fentanyl patches are not for everyone. They are strictly for:- Patients with chronic, around-the-clock pain
- Those already tolerant to opioids (meaning they’ve been taking regular opioid painkillers for at least a week)
They are absolutely not safe for:
- People with acute pain (like after surgery)
- Opioid-naïve patients (those who’ve never taken opioids)
- Children or teenagers
- People with breathing problems like sleep apnea
The FDA and major medical groups have repeatedly warned against using these patches outside of strict guidelines. The dose in one patch can be lethal to someone without opioid tolerance.
What You Need to Do to Stay Safe
If you’re prescribed a fentanyl patch, here’s your action list:- Never use heat sources - no heating pads, hot tubs, saunas, or sunlamps.
- Keep your body temperature normal. Avoid intense exercise, especially in hot weather.
- Check your temperature if you feel sick. Call your doctor if you have a fever.
- Tell every doctor, dentist, or nurse you see that you’re using a fentanyl patch - even for a simple procedure.
- Review all your other medications with your pharmacist. Ask if any interfere with fentanyl metabolism.
- Remove the patch exactly 72 hours after applying it. Don’t leave it on longer.
- Dispose of used patches safely: fold sticky side in, flush or throw away in child-proof container.
- Keep naloxone (Narcan) on hand if you live alone or have someone who cares for you. Know how to use it.
There’s no such thing as a "safe" amount of heat with a fentanyl patch. Even a little extra warmth can tip the balance from treatment to tragedy.
Can I use a fentanyl patch if I have a fever?
No. A fever raises your body temperature, which increases how fast fentanyl is absorbed through your skin. This can lead to dangerous levels of the drug in your blood and cause respiratory depression. Call your doctor immediately if you develop a fever while using a fentanyl patch. Do not wait to see if it gets better.
How long does fentanyl stay in my body after I remove the patch?
Even after you remove the patch, fentanyl continues to be absorbed from your skin for up to 24 hours. This means you’re still at risk for overdose during this time - especially if you’re exposed to heat, exercise, or fever. Never assume the danger ends when you peel off the patch.
Can I use a heating pad if I only wear the patch for a few hours?
No. Fentanyl begins absorbing as soon as the patch is applied. Even short-term heat exposure can cause a rapid spike in blood levels. The patch is designed to work over 72 hours - any heat, at any time, increases the risk of overdose. There is no safe window for heat exposure.
Are there safer alternatives to fentanyl patches?
Yes. For chronic pain, alternatives include long-acting oral opioids like morphine or oxycodone, non-opioid pain relievers like gabapentin or duloxetine, nerve blocks, physical therapy, or spinal cord stimulators. Talk to your doctor about whether a non-transdermal option might be safer for you, especially if you’re at risk for heat exposure or have other health conditions.
Why are fentanyl patches still used if they’re so dangerous?
They’re effective for people who need continuous pain relief and can’t take pills - like those with swallowing difficulties or nausea from cancer. When used exactly as directed - no heat, no other opioids, proper dosing - they’re a valuable tool. The danger comes from misuse, lack of education, or ignoring warnings. The risk is real, but it’s preventable with strict adherence to safety rules.
Can I drink alcohol while using a fentanyl patch?
No. Alcohol increases the sedative effects of fentanyl and can lead to dangerous breathing problems. Even one drink can be risky. Avoid alcohol completely while using the patch and for at least 24 hours after removing it.
What should I do if I accidentally expose my patch to heat?
Remove the patch immediately. Call your doctor or go to the nearest emergency room. Do not wait for symptoms to appear. Tell them you were exposed to heat while using a fentanyl patch. Early intervention can save your life.
Is it safe to use fentanyl patches with other pain medications?
Only if your doctor specifically says so. Combining fentanyl with other opioids, benzodiazepines, sleep aids, or muscle relaxants greatly increases the risk of overdose. Even over-the-counter painkillers like tramadol can interact dangerously. Always review all medications with your pharmacist and prescriber.
Chris Vere
November 22, 2025 AT 05:57It's fascinating how something so simple as heat can unravel a carefully engineered medical system. The body isn't just a container for drugs-it's a living, breathing feedback loop. When we ignore that, we pay the price. I've seen people treat patches like they're batteries-put it on, forget it, wait for relief. But biology doesn't work like that. It’s not magic. It’s physics. And physics doesn't care about your intentions.
Pravin Manani
November 22, 2025 AT 23:43The pharmacokinetic implications of transdermal fentanyl under hyperthermic conditions are non-trivial. The dermal absorption rate increases exponentially with skin temperature due to vasodilation and enhanced membrane fluidity. CYP3A4 inhibition compounds this by reducing first-pass hepatic clearance. Clinically, this creates a dangerous positive feedback loop where even mild pyrexia can precipitate opioid-induced respiratory depression. Patients must be educated not just on heat sources but on metabolic interactions-many are unaware that their antifungal or antibiotic regimen could be lethal in combination.
Leo Tamisch
November 24, 2025 AT 08:14So… let me get this straight. You’re telling me I can’t take a hot shower after getting my fentanyl patch? 😭
And I thought my morning routine was already too strict. Next they’ll tell me not to breathe too hard.
Also, why is this even a thing? Like, who thought this was a good idea? 🤡
Daisy L
November 25, 2025 AT 13:17THIS IS WHY WE NEED TO STOP LETTING PHARMA COMPANIES GET AWAY WITH THIS! THEY MAKE THESE PATCHES LOOK LIKE MAGIC WANDS-'Just stick it on and forget it!'-and then when people die? Oh, it’s 'user error.' NO. IT’S CORPORATE NEGLIGENCE! THEY KNEW HEAT WOULD CAUSE THIS! THEY KNEW! AND THEY DIDN’T EVEN PUT A BIG RED WARNING ON THE BOX! 😡
My cousin died from this. He used a heating pad for his back. He was 42. He had a 6-year-old. And now? No one even talks about it. Because it’s 'just an opioid.' WELL, IT’S NOT JUST AN OPIOID. IT’S A TIME BOMB WITH A STICKY BACKING.
Anne Nylander
November 25, 2025 AT 22:04omg i had no idea about the heat thing!! i thought it was just about not taking too many!!
thank you for this post!! i’m gonna share this with my mom shes on one and she loves her hot tub 😭
also i just called my dr and they said to keep naloxone in the house!! i didnt even know that was a thing!!
Franck Emma
November 27, 2025 AT 06:24One patch. One shower. One death.
That’s it.
That’s the whole story.
Noah Fitzsimmons
November 27, 2025 AT 08:15Wow. So the solution to a drug that’s dangerous when heated… is to tell people not to get warm? What a brilliant innovation. Next we’ll ban people from existing near fire. Or sunlight. Or breathing. Maybe we should just give everyone a thermometer and a handcuff to lock their hands to their sides. Genius. Truly.
Also, you didn’t mention that the FDA approved this in 1990. So… congrats, everyone. We’ve been doing this wrong for 34 years.
Eliza Oakes
November 28, 2025 AT 02:29Okay but what if I’m just cold? Do I just freeze? Do I wear 17 layers? Do I sit in a dark room with no windows? What if I have arthritis and my joints ache? What if I’m a cancer patient and I’m already miserable? Are you saying I have to suffer MORE because some patch can’t handle 98.6°F? That’s not safety. That’s cruelty disguised as caution.
Corra Hathaway
November 28, 2025 AT 03:33Y’all need to chillllll 😌
Yes, heat is dangerous. Yes, this is serious. But don’t panic. Just be smart. Talk to your doc. Ask questions. Use naloxone if you have it. And if you’re worried? Swap to a pill. There are options!!
You’re not alone. You’re not broken. You’re just learning. And that’s okay 💪❤️
Also-don’t forget to hydrate. Water helps your body process everything better.
Shawn Sakura
November 29, 2025 AT 15:32Thank you for this detailed and vital information. I am a caregiver for my father who uses a fentanyl patch for metastatic cancer pain. I had no idea about the 24-hour residual absorption or the CYP3A4 interactions. I have already reviewed his medication list with our pharmacist and removed his electric blanket. I will keep naloxone on hand and ensure all medical personnel are aware. This post has saved lives-including his. Please continue sharing knowledge like this. It matters more than you know.