For millions of people with seasonal or year-round allergies, antihistamines and nasal sprays only offer temporary relief. What if you could actually change how your body reacts to pollen, dust mites, or pet dander - not just mask the symptoms? That’s the promise of immunotherapy, the only allergy treatment proven to retrain your immune system over time.
What Is Immunotherapy, Really?
Immunotherapy isn’t another pill you take when you feel sneezy. It’s a long-term treatment that exposes your body to tiny, controlled amounts of the things you’re allergic to - like grass pollen, ragweed, or house dust mites - so your immune system learns not to overreact. Think of it like a vaccine, but for allergies.
This approach has been around since 1911, when doctors in London first started injecting patients with allergen extracts. Today, it’s backed by decades of research and recommended by major medical groups like the American College of Allergy, Asthma & Immunology (ACAAI). The goal? To reduce or even eliminate allergic reactions for years after treatment ends.
There are two main ways to do this: allergy shots (subcutaneous immunotherapy) and sublingual tablets. Both work on the same principle, but they’re very different in practice.
Allergy Shots: The Gold Standard
Allergy shots - or subcutaneous immunotherapy (SCIT) - are the most effective option for most people with multiple allergies. You get a small injection under the skin, usually in the arm, with a mix of allergens you’re sensitive to. Most people are allergic to more than one thing - 78% are - and shots can target up to four allergens in a single vial.
The process has two phases. First, the build-up phase: you get shots once or twice a week for several months, slowly increasing the dose until you reach the maintenance level. Traditional build-up takes 3 to 12 months. But now, many clinics offer cluster immunotherapy - four to five shots in one visit, repeated weekly - cutting build-up time to just 4 to 9 weeks.
Once you hit maintenance, you switch to shots every 2 to 4 weeks, then eventually every month. You’ll keep this up for 3 to 5 years. That’s a long time, but the results can be life-changing. Studies show 82% of patients on allergy shots see major symptom reduction, and 85% report significant improvement after three years.
Why do they work so well? They trigger your body to produce blocking antibodies that stop the allergic response before it starts. Over time, your immune system stops seeing harmless pollen or dust as a threat. Some patients even stop developing new allergies or avoid progressing to asthma.
Sublingual Tablets: Convenience Over Coverage
Sublingual immunotherapy (SLIT) tablets are the newer, more convenient option. Instead of shots, you place a small tablet under your tongue every day. It dissolves slowly, releasing allergen extracts that your immune system absorbs through the mouth lining.
The FDA has approved four tablets so far: Oralair and Grastek for grass pollen, Ragwitek for ragweed, and Odactra for house dust mites. Each targets just one allergen. That’s the big catch. If you’re allergic to both ragweed and dust mites, you’d need two different tablets - and there’s no combo product available yet.
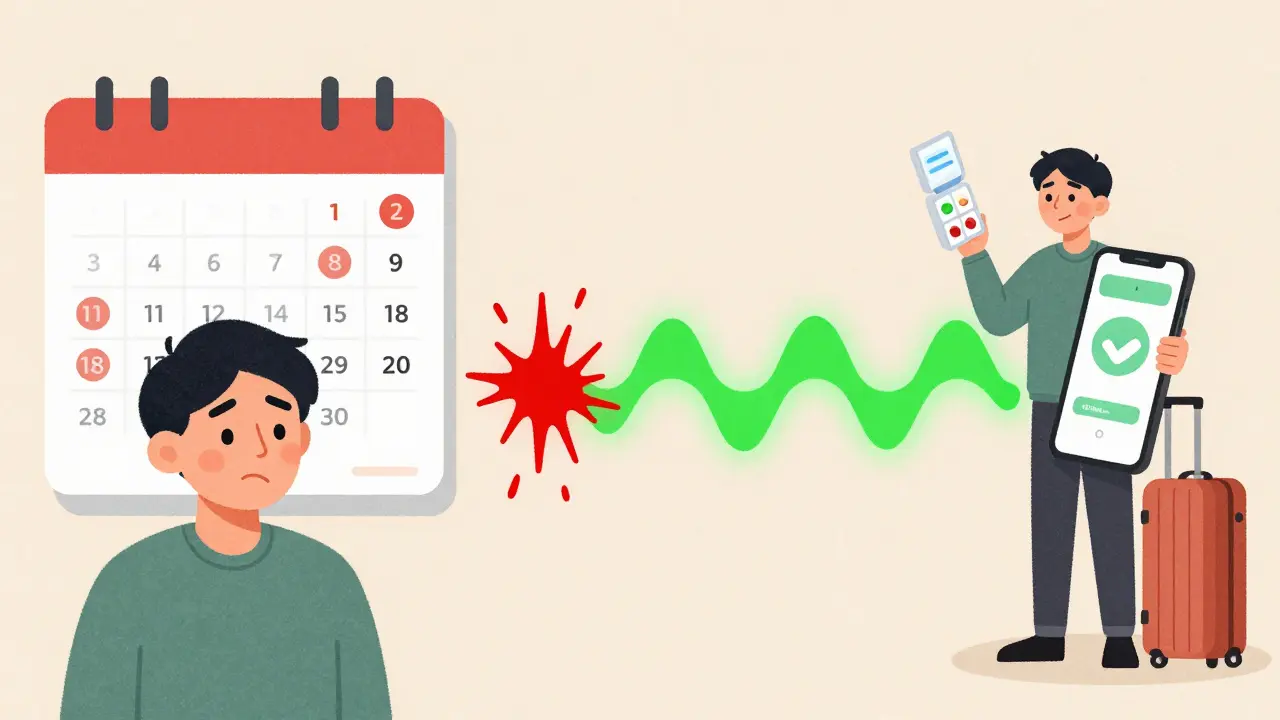
Dosing schedules vary. Oralair is taken daily for 4 months before and during pollen season. Ragwitek and Odactra are taken year-round. You don’t need to visit a clinic. You can take the tablet at home, at work, or while traveling.
But effectiveness drops if you miss doses. Studies show that patients taking less than 80% of their prescribed tablets see only 45% symptom improvement. That’s why adherence is critical. Many people use phone reminders - and those who do improve adherence by 37%.
Overall, SLIT tablets reduce symptoms by about 67% in clinical trials - lower than shots. They’re best for people with one or two specific allergies who can’t handle weekly office visits.

Which One Is Right for You?
There’s no one-size-fits-all answer. Your choice depends on your allergies, lifestyle, and tolerance for inconvenience.
Choose allergy shots if:
- You’re allergic to three or more allergens
- Your symptoms are severe and not controlled by medication
- You want the highest possible chance of long-term relief
- You can commit to weekly or bi-weekly visits for several months
Choose sublingual tablets if:
- You’re allergic to just one or two allergens (like grass or dust mites)
- You travel often or can’t make regular doctor visits
- You hate needles or have a fear of injections
- You’re disciplined enough to take a pill every single day
One Reddit user, who tried both, said: “After 2 years of Grastek tablets with only 30% improvement, I switched to shots and achieved 80% symptom reduction by year 2.” That’s not uncommon. But another user, a traveling salesperson, said: “I couldn’t manage weekly shots, but the tablet fits perfectly in my routine.”
Both groups are right - because both treatments serve different needs.
Safety and Side Effects
Allergy shots carry a small risk of allergic reactions. Most are mild - redness, swelling at the injection site. But in rare cases, they can cause anaphylaxis. That’s why you’re required to wait 30 minutes after each shot. Cluster and rush protocols have slightly higher reaction rates, but modern clinics are well-equipped to handle them.
Sublingual tablets are safer overall. The most common side effect is mild itching or tingling under the tongue - affecting about 28% of users. Serious reactions are extremely rare. But because you take them at home, you need to know the warning signs of a severe reaction and have an epinephrine auto-injector on hand if your doctor recommends it.
Neither treatment is risk-free, but both are far safer than long-term reliance on steroids or daily antihistamines.
Cost, Accessibility, and the Future
Allergy shots cost more upfront - $1,500 to $4,000 over 3-5 years - but most insurance plans cover them. Sublingual tablets cost $1,200 to $2,000 annually, and coverage varies. Some patients pay out-of-pocket because their insurance doesn’t cover SLIT.
Access is another issue. There are only about 5,300 board-certified allergists in the U.S. - not nearly enough to meet demand. In rural areas, getting shots can mean driving hours. That’s why sublingual tablets are growing fast, even with their limitations.
The future is promising. In April 2024, the FDA approved the first tablet for cat dander allergy (Cat-PAD). More multi-allergen tablets are in Phase 3 trials and could hit the market by 2025. Researchers are also testing peptide-based therapies that could cut treatment time from 3-5 years to just 1-2.
What’s clear is that immunotherapy is becoming more personalized. Allergists are now using component-resolved diagnostics to match patients with the exact proteins causing their allergies - not just broad allergen extracts. That means better results and fewer side effects down the road.
Real Talk: What Patients Actually Experience
On Google reviews, the most common phrase about allergy shots is “life-changing after two years.” On Amazon, the top comment about sublingual tablets is “convenient and easy to use.”
But here’s the truth: most people who quit immunotherapy don’t do it because it doesn’t work - they quit because it’s hard to stick with. Shots require time. Tablets require discipline.
If you’re serious about getting off the allergy medication treadmill, you need to pick the method that fits your life - not the one that sounds easier. A 2022 survey found that 63% of people who stopped shots did so because they couldn’t fit appointments into their schedule. Another 41% quit because of injection discomfort.
For tablets, 58% of negative reviews cite poor results - mostly because they were used by people with multiple allergies. The tablet isn’t broken. It’s just not designed for them.
Getting Started
If you think immunotherapy might help you:
- See an allergist for testing. Skin or blood tests will identify exactly what you’re allergic to.
- Discuss your lifestyle. Can you commit to weekly visits? Do you forget to take pills?
- Ask about cluster immunotherapy. It’s faster and just as safe as traditional build-up.
- Check your insurance. Coverage varies, but most plans cover shots and some cover tablets.
- Start early. The sooner you begin, the sooner you’ll see results - and the more you’ll save on years of daily meds.
Immunotherapy isn’t a quick fix. But for many, it’s the only real cure.
Are allergy shots worth the time and effort?
Yes - if you have multiple allergies or severe symptoms. Allergy shots are the most effective treatment available, with 82-85% of patients seeing major improvement after 3 years. The time investment is real - weekly visits for months - but the payoff is long-term relief, fewer medications, and often, prevention of new allergies or asthma.
Can sublingual tablets treat multiple allergies?
Not yet. Current FDA-approved tablets only target one allergen at a time: grass, ragweed, dust mites, or cat dander. If you’re allergic to more than one, you’d need multiple tablets - and there’s no combination product on the market. That’s why shots remain the only option for comprehensive treatment.
How long before I see results from immunotherapy?
Most people start noticing improvement within 6 to 12 months. But full benefits take 2 to 3 years. Don’t expect miracles after a few weeks. Immunotherapy works by slowly retraining your immune system. The longer you stick with it, the better the results - and the longer the relief lasts after treatment ends.
Is immunotherapy safe for children?
Yes. Both allergy shots and sublingual tablets are approved for children as young as 5. In fact, starting early can prevent the progression of allergies into asthma. Pediatric allergists often recommend immunotherapy for kids with moderate to severe allergic rhinitis who don’t respond well to medication.
Do I have to take immunotherapy forever?
No. The standard course is 3 to 5 years. After that, most patients maintain their improved tolerance for years - sometimes permanently. Studies show that 70-80% of people stay symptom-free for at least 10 years after stopping treatment. You’re not on it for life - just long enough to reset your immune system.

Neil Ellis
January 23, 2026 AT 00:42Man, I wish I’d known about this stuff 10 years ago. I used to live in a cloud of tissues and Sudafed every spring - now I’m 90% symptom-free after three years of shots. It’s not glamorous, but neither is sneezing through your kid’s soccer games. Worth every minute. 🌿💪
Rob Sims
January 24, 2026 AT 08:12Oh please. Another ‘immunotherapy is magic’ post. You know what’s *really* changing people’s lives? Moving to a desert. No pollen. No dust mites. No need to inject yourself or swallow pills like a lab rat. Just move to Arizona. Problem solved. 🏜️
Mike P
January 26, 2026 AT 06:51LOL you think moving to Arizona fixes everything? Bro, I’ve got dust mites in my *bedroom* and cat dander on my couch - Arizona’s sand doesn’t help when your cat’s got a 12-pound fur coat. And yeah, shots are a hassle, but I’d rather drive 45 minutes once a month than spend my life on Zyrtec like a zombie. This isn’t a lifestyle upgrade - it’s a medical necessity. Stop being lazy and get tested.
Daphne Mallari - Tolentino
January 28, 2026 AT 06:23While the clinical efficacy of subcutaneous immunotherapy is well-documented in peer-reviewed literature, one must acknowledge the profound sociological implications of its adoption. The commodification of immune modulation - wherein patients are coerced into long-term, clinic-dependent regimens - reflects a broader pathology within contemporary healthcare systems. One wonders whether the true beneficiary is the patient… or the pharmaceutical-industrial complex. 🤔
Akriti Jain
January 28, 2026 AT 23:04Wait… so you’re telling me Big Pharma doesn’t want us to cure allergies? 😏 They make billions off antihistamines… and now they give us ‘tablets’ that only work for ONE thing? Coincidence? I think not. 🤫🧪 #AllergyConspiracy #TheyWantYouSneezing
arun mehta
January 29, 2026 AT 17:09Respectfully, the science behind immunotherapy is both elegant and profoundly humane. It is not a commercial gimmick but a restoration of physiological equilibrium. For millions, especially children in developing nations where allergic rhinitis progresses to asthma, this is not a luxury - it is a lifeline. Let us not reduce medical progress to cynicism, but celebrate the quiet revolution in immunology that allows one to breathe freely again. 🌏❤️
Patrick Roth
January 29, 2026 AT 22:39Actually, in Ireland we’ve had sublingual tablets available since 2015, and they’re covered by the public health system. Here, shots are seen as ‘old school.’ And guess what? We don’t have a single allergist shortage. Maybe it’s not the treatment - maybe it’s your healthcare system that’s broken. Just saying.
Chiraghuddin Qureshi
January 30, 2026 AT 17:01My cousin in Delhi used to sneeze for 8 months a year. Got sublingual tablets for dust mites - took 4 months to notice, now he’s playing cricket in May without a tissue. No shots. No drama. Just consistency. 🌏🙏