Cholesterol Medication LDL Reduction Calculator
Your Current LDL Level
Enter your current LDL cholesterol level (in mg/dL) to estimate potential reduction.
Estimated LDL Reduction
Important Note: Your actual reduction may vary based on individual factors including genetics, diet, and other medications.
What You Really Need to Know About PCSK9 Inhibitors and Statins
If you’ve been told your cholesterol is too high and you’re trying to figure out whether to stick with statins or switch to a PCSK9 inhibitor, you’re not alone. Millions of people face this exact choice every year. The truth? These two drugs work in completely different ways, have very different side effects, and aren’t really meant to replace each other - they’re often used together. But understanding the differences can make all the difference in your health and quality of life.
Statins have been the go-to for over 35 years. They’re cheap, well-studied, and work for most people. But for those who can’t tolerate them - or who still have dangerously high LDL even on high doses - PCSK9 inhibitors offer a powerful alternative. The key isn’t just which one is stronger. It’s which one fits your body, lifestyle, and risk level.
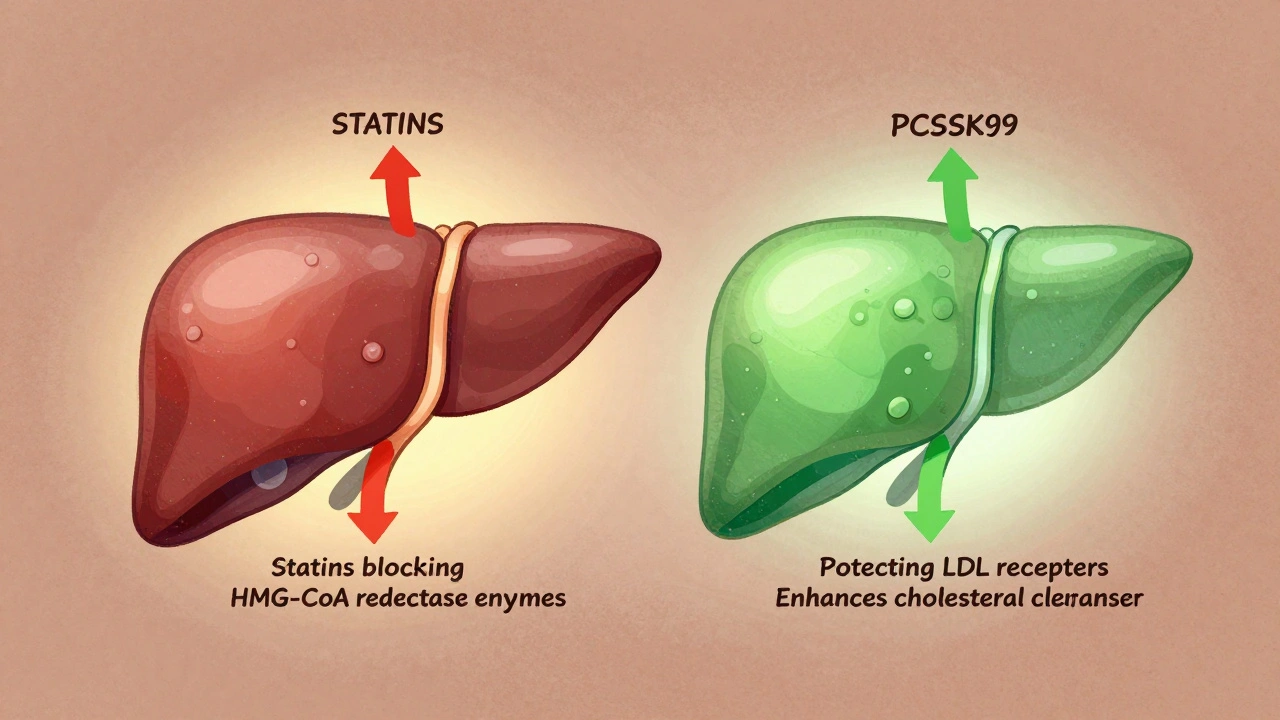
How Statins Actually Work (And Why They’re Still First-Line)
Statins don’t just lower cholesterol - they stop your liver from making it in the first place. They block an enzyme called HMG-CoA reductase, which is the main step your body uses to produce LDL, the "bad" cholesterol. That’s why they’re so effective: they cut production at the source.
Most statins are taken once a day, usually in the evening, because your liver makes the most cholesterol at night. Common ones include atorvastatin (Lipitor), rosuvastatin (Crestor), and simvastatin (Zocor). High-intensity statins like these can drop LDL by 50% or more. For someone with a 180 mg/dL LDL, that means bringing it down to around 90 - which might be good enough.
But here’s the catch: statins don’t work the same for everyone. About 1 in 10 people get muscle pain or weakness. For some, it’s mild. For others, it’s so bad they have to stop. That’s called statin intolerance. And it’s not just muscle pain - some people report brain fog, fatigue, or even elevated liver enzymes. These aren’t rare side effects. They’re common enough that doctors routinely check liver enzymes and ask about muscle symptoms after starting a statin.
Still, statins have something no other cholesterol drug can match: decades of proof they save lives. Large studies show they reduce heart attacks, strokes, and death in people with heart disease - and even in people at high risk who haven’t had an event yet. That’s why guidelines still say: start with a statin.
PCSK9 Inhibitors: The New Kid on the Block
PCSK9 inhibitors are something else entirely. They don’t touch cholesterol production. Instead, they help your liver clear more LDL from your blood. How? By blocking a protein called PCSK9, which normally destroys LDL receptors on liver cells. When you block PCSK9, those receptors stick around longer - and they pull more LDL out of your bloodstream.
There are two main ones: alirocumab (Praluent) and evolocumab (Repatha). Both are injected under the skin, either every two weeks or once a month. They’re not pills. You can’t just pop one with your morning coffee. You need to learn how to give yourself a shot. Most people get the hang of it after one or two tries.
And the numbers? They’re impressive. In clinical trials, PCSK9 inhibitors lower LDL by 50-61%. That’s more than most statins can do. For someone with an LDL of 200 mg/dL, a PCSK9 inhibitor might bring it down to 80 or even 60. That’s the kind of drop that matters for people with familial hypercholesterolemia or a history of heart attack or stroke.
What’s more, they don’t cause muscle pain. In fact, they’re often prescribed to people who had to stop statins because of muscle issues. A 2024 review of over 36 trials found no link between PCSK9 inhibitors and muscle damage. That’s a huge win for patients who’ve been stuck between high cholesterol and unbearable side effects.
Side Effects: What You’ll Actually Feel
Let’s cut through the noise. What do people really experience?
Statins: On Drugs.com, 8,452 users rated statins an average of 6.8 out of 10. The top complaints? Muscle pain (32%), fatigue (21%), and brain fog (18%). Some report digestive issues or sleep problems. Liver enzyme elevations happen in about 1-3% of users - usually mild and reversible. There’s also a small but real increase in hemorrhagic stroke risk in people with prior bleeding in the brain. That’s why doctors avoid high-dose statins in certain patients.
PCSK9 inhibitors: With 1,204 reviews, they score 7.9 out of 10. The biggest praise? "No muscle pain" (79%) and "dramatic LDL drop" (82%). But the complaints are real too: injection anxiety (41%), cost (38%), and insurance battles (33%). Some people get redness or itching at the injection site - but that’s usually temporary. There’s no evidence they cause liver damage, muscle issues, or diabetes. And unlike statins, they don’t increase stroke risk.
One big surprise? PCSK9 inhibitors don’t seem to affect blood sugar or increase diabetes risk - something statins can do in a small percentage of people. That’s important if you’re prediabetic or have metabolic syndrome.
Who Gets Which Drug? The Real-World Rules
Doctors don’t just pick one because it’s "better." They pick based on your risk, your tolerance, and your access.
- If you have heart disease, a prior stroke, or diabetes with other risk factors - start with a high-intensity statin. Add ezetimibe if needed.
- If your LDL stays above 70 mg/dL on maximum tolerated statin therapy - add a PCSK9 inhibitor.
- If you can’t take any statin because of muscle pain - PCSK9 inhibitors are your best bet.
- If you have familial hypercholesterolemia - you’re likely to need both, or even a PCSK9 inhibitor alone.
- If you’re young, healthy, and just have high cholesterol - statins are still the standard. PCSK9 inhibitors are overkill.
And here’s the hard truth: insurance won’t cover PCSK9 inhibitors unless you’ve tried and failed on statins. In the U.S., 87% of insurers require proof of statin intolerance or failure to reach LDL targets before approving them. That means you might need to document muscle pain, lab results, and even a letter from your doctor. It’s a hassle - but it’s the rule.

Cost: The Elephant in the Room
Statins? Generic atorvastatin costs $4 to $10 a month. Even brand-name Crestor is under $30 with coupons.
PCSK9 inhibitors? $5,000 to $14,000 a year. That’s not a typo. But here’s what’s changed: manufacturers now offer copay cards that can bring your monthly cost down to $0-$300. And more insurers are covering them as costs drop and outcomes improve.
Still, the gap is massive. A 2024 analysis found that adding a PCSK9 inhibitor to a statin costs 3.2 times more than adding ezetimibe. That’s why doctors don’t jump to them - they’re not a first-line tool. They’re a targeted tool for high-risk cases where the payoff is clearest: preventing heart attacks and strokes in people who’ve already had one.
What’s Coming Next?
The field is moving fast. In 2021, the FDA approved inclisiran (Leqvio), a PCSK9 inhibitor you only need to inject twice a year. That’s a game-changer for people who hate frequent shots.
Even more exciting? Oral PCSK9 inhibitors are in Phase II trials. Merck’s MK-0616 reduced LDL by 60% in early studies - and it’s a pill. If it gets approved, it could replace injections entirely.
And while statins are aging, they’re not going away. New formulations, better dosing strategies, and combination pills are keeping them relevant. The real future? Personalized medicine. Blood tests to predict who responds best to statins. Genetic testing for familial hypercholesterolemia. Algorithms that calculate your 10-year risk and recommend exactly which drug you need.
Final Take: It’s Not Either/Or - It’s And
Most people don’t need PCSK9 inhibitors. For them, statins work fine. But for the 1 in 10 who can’t tolerate them - or the 1 in 20 who still have dangerous cholesterol levels despite taking them - PCSK9 inhibitors aren’t just an option. They’re a lifeline.
The goal isn’t to pick the "best" drug. It’s to pick the one that gets your LDL to target - safely, sustainably, and without wrecking your daily life. If you’re on a statin and feel fine? Keep going. If you’re struggling with side effects or your numbers won’t budge? Talk to your doctor about PCSK9 inhibitors. Don’t assume they’re out of reach. Ask about copay help. Ask about prior authorization. Ask if you’re a candidate.
Cholesterol isn’t just a number. It’s a signal. And sometimes, the right drug is the one that lets you live without fear - without pain - without compromise.
Can you take PCSK9 inhibitors and statins together?
Yes, and many high-risk patients do. Combining a statin with a PCSK9 inhibitor can lower LDL by up to 75%, which is often needed for people with familial hypercholesterolemia or a history of heart attack. This combination is safe and commonly used when statins alone aren’t enough.
Do PCSK9 inhibitors cause muscle pain like statins?
No. PCSK9 inhibitors do not cause statin-like muscle pain or damage. In fact, they’re often prescribed specifically to patients who developed muscle symptoms from statins. Clinical trials show no increase in muscle-related side effects compared to placebo.
Are PCSK9 inhibitors better than statins for stroke prevention?
They’re safer for certain types of stroke. Statins slightly increase the risk of hemorrhagic stroke in people with a history of brain bleeding. PCSK9 inhibitors show no such risk in large trials. For those patients, PCSK9 inhibitors may be the preferred option - especially if LDL is still too high.
How long does it take for PCSK9 inhibitors to work?
You’ll see LDL reductions within weeks. Most patients reach their lowest LDL level after 4 to 8 weeks of treatment. Unlike statins, which can take a few weeks to build up, PCSK9 inhibitors act quickly because they directly increase LDL receptor activity in the liver.
Is there a cheaper alternative to PCSK9 inhibitors?
Yes. Ezetimibe (Zetia) is a pill that lowers LDL by about 15-20% and costs under $20 a month. It’s often added to statins before moving to a PCSK9 inhibitor. Another option is bempedoic acid (Nexletol), which works similarly to statins but with less muscle risk. Both are much cheaper and easier to access.
Can I stop taking statins if I start a PCSK9 inhibitor?
Sometimes - but not always. Many doctors keep patients on a low-dose statin even when adding a PCSK9 inhibitor, because statins have anti-inflammatory effects that may help stabilize artery plaques. Stopping statins entirely should only be done under medical supervision, especially if you have heart disease.
Do PCSK9 inhibitors need refrigeration?
Yes. Both alirocumab and evolocumab must be stored in the refrigerator until use. They can be kept at room temperature for up to 14 days if needed, but should not be exposed to heat or direct sunlight. Always check the package insert for exact storage instructions.
How often do I need to inject PCSK9 inhibitors?
Alirocumab (Praluent) is usually injected every two weeks. Evolocumab (Repatha) can be injected either every two weeks or once a month, depending on the dose. Your doctor will decide based on your LDL levels and insurance coverage.
soorya Raju
December 1, 2025 AT 15:48Lucinda Bresnehan
December 2, 2025 AT 12:57Kshitij Shah
December 3, 2025 AT 12:05Sean McCarthy
December 3, 2025 AT 13:38Jaswinder Singh
December 5, 2025 AT 08:52Courtney Co
December 6, 2025 AT 22:09Souvik Datta
December 8, 2025 AT 13:20Irving Steinberg
December 9, 2025 AT 19:23Kay Lam
December 11, 2025 AT 03:04Matt Dean
December 13, 2025 AT 00:08Walker Alvey
December 14, 2025 AT 20:43Adrian Barnes
December 16, 2025 AT 11:03