For many people living with rheumatoid arthritis (RA), the daily pain, stiffness, and swelling aren’t just inconvenient-they’re life-limiting. But over the last 25 years, a new wave of treatments has changed the game. Biologic DMARDs aren’t just another pill or injection. They’re precision tools designed to quiet the immune system’s attack on your joints. And for a growing number of patients, they’re the key to something once thought impossible: true disease remission.
What Are Biologic DMARDs, Really?
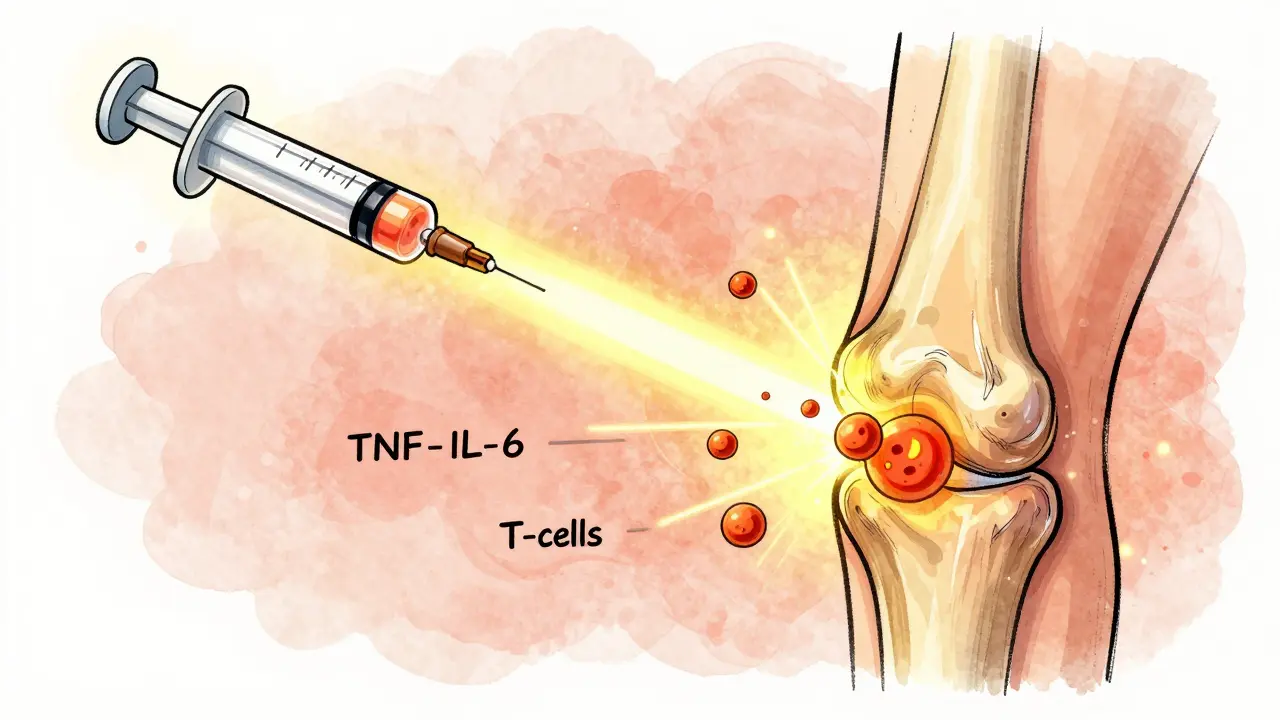
Biologic DMARDs (disease-modifying antirheumatic drugs) are made from living cells, not chemicals. Unlike older drugs like methotrexate that broadly suppress the immune system, biologics target specific troublemakers-like TNF-alpha, IL-6, or T-cells-that drive RA inflammation. Think of it like using a sniper instead of a shotgun.
The first one, etanercept (Enbrel), hit the market in 1998. Since then, we’ve seen a whole family of these drugs emerge. TNF inhibitors include adalimumab (Humira), infliximab (Remicade), and golimumab (Simponi). Then there are non-TNF options like abatacept (Orencia), which blocks T-cell activation, rituximab (Rituxan), which wipes out B-cells, and tocilizumab (Actemra), which shuts down IL-6 signaling. JAK inhibitors like tofacitinib (Xeljanz) and upadacitinib (Rinvoq) are technically synthetic, but they work the same way-targeting specific immune signals inside cells.
These aren’t just lab experiments. They’re used by hundreds of thousands of people worldwide. In the U.S. and Western Europe, about 25-30% of RA patients are on a biologic. That number jumps to over 60% for those who didn’t respond to methotrexate alone.
How Do Biologics Compare to Traditional RA Drugs?
Methotrexate is still the first step for most people. It’s cheap, well-studied, and works for many. But here’s the catch: about 40-50% of patients don’t get enough relief from it. That’s when biologics come in.
Studies show that when you add a biologic to methotrexate-or use it alone-20-50% of patients reach remission. Compare that to just 5-15% with methotrexate alone. That’s not a small improvement. That’s a game-changer.
And it’s not just about feeling better. X-rays tell the real story. People on biologics show far less joint damage over time. One 2022 study found that patients on adalimumab or etanercept had 19% less joint erosion progression than those on infliximab. That’s not just comfort-it’s preserving your ability to walk, grip, and live independently.

Which Biologic Works Best?
There’s no one-size-fits-all. What works for your neighbor might not work for you. But research gives us some clear patterns.
- TNF inhibitors (adalimumab, etanercept, infliximab) are the most common. They work fast-sometimes in days. But in real-world data, non-TNF drugs like tocilizumab and abatacept often outperform them.
- Tocilizumab (Actemra) is especially effective in people with high IL-6 levels. One study found 50% of patients with certain biomarkers responded to it, while only 12% responded to rituximab.
- Abatacept (Orencia) and rituximab (Rituxan) are good choices if you’ve tried TNF blockers and failed. They work differently, so they can still help.
- JAK inhibitors like upadacitinib and baricitinib have shown higher remission rates than older biologics in head-to-head trials. In fact, baricitinib achieved 28% higher remission rates than traditional biologics in one 2023 cohort study.
And here’s something many don’t realize: switching between biologics doesn’t always help. If you’ve tried two or three, your chances of responding to a fourth drop sharply. That’s why experts now say: choose wisely the first time. It’s not about trying everything-it’s about matching the drug to your body’s biology.
Real People, Real Results
On patient forums, the stories are powerful. One woman in her 50s, who hadn’t been able to open a jar in 10 years, started tocilizumab and could grip her coffee cup again within 8 weeks. Another man, who used a cane for years, got off it after switching to adalimumab.
But it’s not all success. About 30% of people don’t respond at all to their first biologic. And 40% of those who do respond eventually lose effectiveness after 1-2 years. That’s called secondary non-response. It’s frustrating, but it’s normal. It doesn’t mean you failed-it means your disease evolved.
Side effects are real. Injection site reactions are common-45% of reports mention redness or itching. Infections are the big concern. Biologics raise your risk of pneumonia, tuberculosis, and other serious infections. That’s why doctors test for TB before starting any of them. And yes, they cost a lot. In the U.S., they run $50,000-$70,000 a year. But biosimilars-copies of the original drugs-are now available and cut costs by 15-30%. Many patients on biosimilars report the same results at lower prices.
What You Need to Know Before Starting
If you’re considering a biologic, here’s what matters:
- Training matters. Most biologics are injected under the skin. With two training sessions, 75% of patients can do it themselves. You’ll learn how to store them, how to rotate injection sites, and how to handle the device.
- Timing matters. You won’t feel better overnight. TNF inhibitors can work in 2-4 weeks. Others take 3-6 months. Don’t give up too soon.
- Monitoring matters. Your doctor will check your blood, watch for infections, and use tools like DAS28 (a score based on joint swelling, pain, and lab markers) to track progress.
- Support matters. Most drugmakers offer patient assistance programs that cover 40-100% of costs. Specialty pharmacies handle delivery and education. Tools like ArthritisPower or MyRApath help you log symptoms and track progress.
The Future: Personalized RA Treatment
The next big shift isn’t just more drugs-it’s smarter choices. Researchers are now using synovial tissue biopsies to see what’s happening inside your joints. If your joint has lots of B-cells, rituximab might be perfect. If it’s full of IL-6 signals, tocilizumab could be the answer. This isn’t science fiction-it’s happening now in research centers.
Longer-lasting injections are coming too. A twice-yearly version of tocilizumab is in Phase III trials. That means fewer trips to the clinic and less hassle.
And biosimilars? They’ll keep growing. By 2027, they’re expected to make up 60% of the biologic market. That’s good news for patients and healthcare systems alike.
Remission isn’t a miracle anymore. It’s a realistic goal. But it takes patience, the right drug, and ongoing care. You’re not just treating pain-you’re protecting your joints, your independence, and your future.
Can biologic DMARDs cure rheumatoid arthritis?
No, biologic DMARDs don’t cure rheumatoid arthritis. But they can put the disease into remission-meaning little to no active inflammation, no joint damage progression, and minimal symptoms. Many people stay in remission for years while on treatment. Stopping the drug often leads to a return of symptoms, so most patients continue therapy long-term.
How long does it take for biologics to start working?
It varies. TNF inhibitors like adalimumab or etanercept often show improvement in 2-4 weeks. Non-TNF biologics like abatacept or tocilizumab can take 3-6 months to reach full effect. Patience is key-don’t stop because you don’t feel better right away. Your doctor will track your progress with blood tests and joint exams.
Are biosimilars as effective as the original biologics?
Yes. Biosimilars are highly similar to the original biologic drugs in structure, function, and clinical effect. Studies show they work just as well for RA. The main difference is cost-biosimilars are typically 15-30% cheaper. Many patients switch successfully without losing symptom control. Always talk to your rheumatologist before switching.
What are the biggest risks of biologic DMARDs?
The biggest risk is serious infections, including tuberculosis, pneumonia, and fungal infections. Before starting, you’ll be tested for TB and hepatitis. Other risks include increased risk of certain cancers (like lymphoma), though the absolute risk remains low. Injection site reactions are common but usually mild. Always report fever, chills, or unexplained fatigue to your doctor right away.
Can I stop taking methotrexate if I start a biologic?
Sometimes, but not usually. Most rheumatologists recommend continuing methotrexate with a biologic because the combination works better than either alone. It improves response rates and reduces the chance your body will develop antibodies against the biologic. But if you can’t tolerate methotrexate, biologics can be used alone-with slightly lower effectiveness.
Why do some people stop responding to biologics over time?
This is called secondary non-response. It happens in about 40% of patients after 12-24 months. The reasons aren’t fully understood, but your immune system may start making antibodies against the drug, or your disease may shift to use different inflammatory pathways. That’s why switching to a biologic with a different target-like going from a TNF inhibitor to an IL-6 blocker-can restore control.
Is there a way to predict which biologic will work for me?
Not yet in routine practice, but research is close. Scientists are using joint tissue biopsies and blood biomarkers to match patients to drugs. For example, if your joint has high B-cell activity, rituximab is more likely to work. If IL-6 is dominant, tocilizumab is better. These tools are still in clinical trials but could become standard in the next 5-10 years.
What should I do if I can’t afford my biologic?
You’re not alone. Most drugmakers offer patient assistance programs that cover 40-100% of costs for qualifying patients. Ask your rheumatologist or pharmacy for help applying. Biosimilars are also significantly cheaper. Specialty pharmacies can help you navigate insurance approvals and copay assistance. Never stop your medication because of cost-talk to your care team first.
Biologic DMARDs didn’t just change how we treat rheumatoid arthritis-they changed what we thought was possible. Remission isn’t a dream anymore. It’s a destination. And with the right drug, the right support, and the right mindset, it’s one you can reach.