Medication Timing Checker
How Medication Timing Affects You
Select your medication below to see how timing impacts effectiveness and side effects. Many drugs work best when taken at specific times due to your body's circadian rhythm.
Select a medication to see timing recommendations
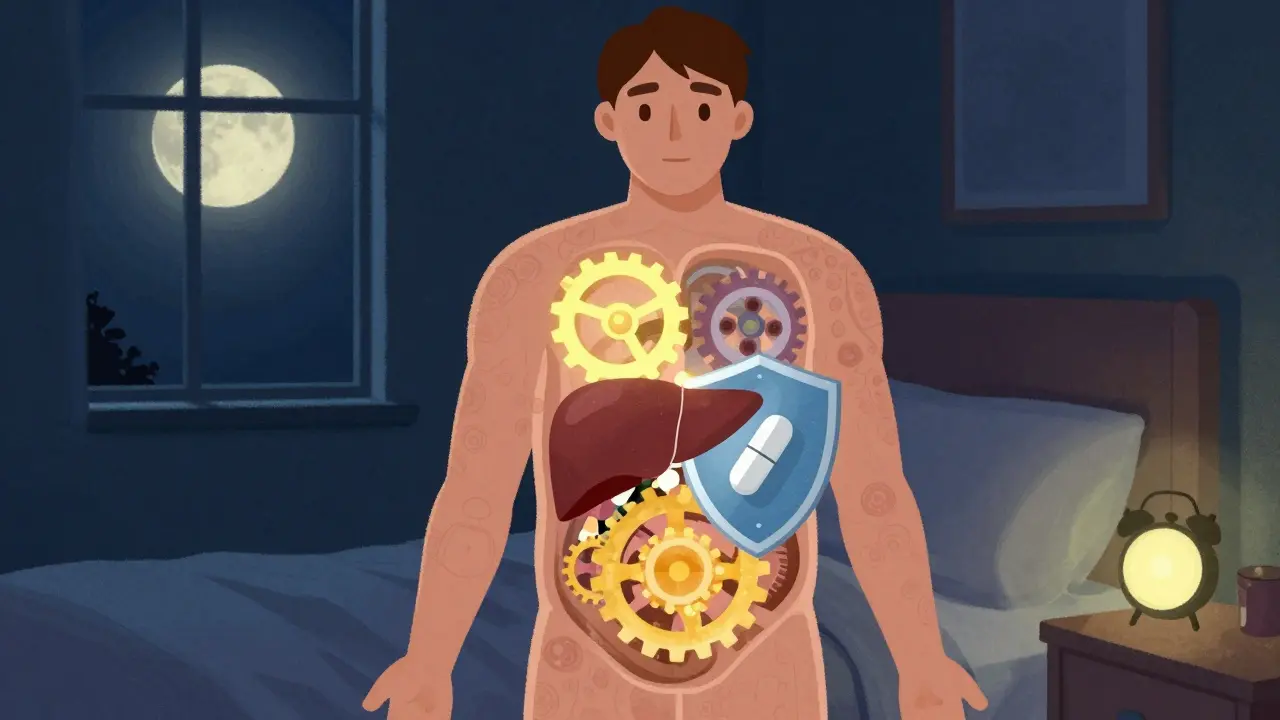
Have you ever wondered why your doctor told you to take your blood pressure pill at night, or your statin before bed? It’s not just a random instruction. The time you take your medication can make a real difference in how well it works-and how badly it might make you feel. Many people assume that as long as they take their pills, the timing doesn’t matter. But science says otherwise. Timing isn’t just a suggestion; it’s a key part of safe, effective treatment.
Why Your Body’s Clock Matters
Your body runs on a 24-hour cycle called the circadian rhythm. It controls sleep, hunger, hormone levels, and even how your liver breaks down drugs. This means the same dose of a medication can behave completely differently depending on whether you take it at 7 a.m. or 7 p.m. For example, cholesterol production in the liver peaks between midnight and 4 a.m. That’s why statins like atorvastatin work better when taken at night. Studies show evening dosing can lower LDL (bad) cholesterol by 15-20% more than morning doses. The drug doesn’t change. Your body does. Same goes for blood pressure meds. A major study called MAPEC found that taking ACE inhibitors at bedtime reduced heart attacks and strokes by 29% compared to morning dosing. Why? Because blood pressure naturally dips at night. Taking the pill then helps maintain that dip, protecting your heart. Take it in the morning, and you might disrupt your body’s natural rhythm-raising your risk of complications.Medications That Need Exact Timing
Not all drugs are created equal when it comes to timing. Some can be taken anytime. Others? Miss the window by even 15 minutes, and things go wrong. Insulin is one of the most timing-sensitive. If you take rapid-acting insulin too early before a meal, you risk low blood sugar. Too late, and your sugar spikes dangerously high. In hospital settings, mistimed insulin leads to hypoglycemia in about 22% of cases. At home, where monitoring is looser, the risk is even higher. Anticoagulants like warfarin or rivaroxaban also demand precision. A delay of just a few hours can throw off your clotting levels. Studies show timing errors increase bleeding risk by up to 37%. That’s not a small number. It’s life-threatening. Chemotherapy drugs are another example. In cancer care, timing isn’t just about comfort-it’s about survival. Deviating from the scheduled window by more than 30 minutes can cut effectiveness by 15-20%. Oncology teams now use strict protocols, sometimes even scheduling infusions around a patient’s natural sleep cycle to reduce nausea and fatigue.What About the Other Drugs?
You might be thinking, “But I take ibuprofen or a multivitamin. Does timing matter?” For many common medications, the answer is no-not much. A dose of hydrochlorothiazide (a water pill) taken 12 hours late won’t hurt you. Same with most antibiotics like amoxicillin. The body can handle some flexibility. But here’s the catch: even “flexible” meds can cause side effects if taken at the wrong time. Take NSAIDs like naproxen. If you take them at night, they can disrupt sleep and raise stomach acid, increasing the chance of ulcers. Take them with food in the morning? Much safer. Even something as simple as thyroid medication (levothyroxine) needs to be taken on an empty stomach, usually first thing in the morning. If you take it with coffee, calcium, or iron-common morning habits-you block absorption. The pill still gets swallowed. But your body doesn’t use it. That’s not a side effect-it’s a treatment failure.
How Timing Errors Happen
You’d think hospitals would get this right. But they don’t always. A study of over 1,600 medication administrations found that nearly 43% had timing errors. Why?- Interruptions during med rounds. Nurses get pulled away for emergencies, phone calls, or paperwork. One study showed that with five interruptions, error rates jumped from 39% to 61%.
- Confusing schedules. A patient on 10 meds might have 5 different times to take them. No one remembers.
- Home life. Shift workers, caregivers with busy jobs, or people without alarms often miss windows. One survey found 68% of patients on chronotherapy meds couldn’t stick to their schedule.
- Technology gaps. Many electronic health records still treat all meds the same-no matter if they’re high-risk or low-risk.
How to Get Timing Right
If you’re on medication, here’s how to make timing work for you-not against you:- Ask your pharmacist: “Is timing important for this drug?” Don’t assume. Some meds need exact windows. Others don’t.
- Use alarms: Set two alarms-one 15 minutes before, one at the time. Phone reminders work better than paper lists.
- Group meds: If you take three pills at night, keep them together in a pillbox labeled “PM.” Same for morning.
- Track your side effects: Keep a simple log: “Took at 8 a.m. → dizzy.” “Took at 10 p.m. → no dizziness.” Patterns matter.
- Use barcode systems: If you’re in a hospital, ask if they use barcode scanning for meds. It cuts timing errors by 28%.

The Future of Timing
This isn’t just about old-school pills anymore. The field is called chronotherapy-and it’s growing fast. In 2023, the FDA started requiring drug makers to include circadian data in new drug applications. Epic’s new ChronoCare module now flags high-risk meds and warns if doses are too early or late. By 2027, experts predict 65% of high-risk drugs will have official timing guidelines. Even more exciting? Research into personalized chronotherapy. The ChronoGene study (ending late 2024) is testing how your genes affect your body’s clock. One person might absorb a drug best at 9 p.m. Another at 11 p.m. Soon, your pill schedule might be as unique as your fingerprint.What This Means for You
Timing isn’t about perfection. It’s about awareness. If your medication causes dizziness, nausea, or fatigue, ask: When am I taking this? A simple shift-moving a pill from morning to night, or vice versa-could cut side effects in half. Don’t wait for your doctor to bring it up. Bring it up yourself. Say: “I’ve been feeling X. Could timing have anything to do with it?” You might be surprised how often the answer is yes. The science is clear: your body’s clock is always ticking. Your meds should match it.Does the time I take my medication really affect side effects?
Yes, for many medications. Your body’s internal clock affects how drugs are absorbed, metabolized, and cleared. For example, taking statins at night reduces LDL cholesterol more effectively and can lower muscle pain side effects. Timing also matters for insulin, blood pressure meds, and anticoagulants-where even small delays can increase risks like hypoglycemia or bleeding.
Which medications are most sensitive to timing?
High-risk medications include insulin, anticoagulants (like warfarin or rivaroxaban), chemotherapy drugs, and certain blood pressure medications (especially ACE inhibitors). These require administration within tight windows-often within 15 to 30 minutes of the scheduled time. Mistiming can lead to serious side effects like low blood sugar, excessive bleeding, or reduced treatment effectiveness.
Can I take my pills at a different time if it’s more convenient?
For some medications, yes. Over-the-counter pain relievers, most antibiotics, and multivitamins are flexible. But for chronic conditions like hypertension, diabetes, or high cholesterol, changing timing without medical advice can reduce effectiveness or increase side effects. Always check with your pharmacist before adjusting your schedule.
Why do some meds work better at night?
Your body’s biological rhythms control how drugs are processed. For example, cholesterol production peaks overnight, so statins taken at night block more of it. Blood pressure naturally dips at night, so taking ACE inhibitors then helps maintain that dip and reduces heart strain. Hormone levels, liver enzyme activity, and kidney filtration all follow daily patterns that affect how drugs behave.
I’m a caregiver. How can I help someone stick to their medication schedule?
Use alarms, pill organizers labeled by time of day, and tie medication to daily routines like brushing teeth or eating breakfast. Avoid relying on memory alone. If the person works night shifts or has irregular hours, talk to their doctor about adjusting the schedule. Many medications can be safely taken at different times if done consistently.
Do hospitals and pharmacies have systems to help with timing?
Yes. Hospitals use barcode scanning systems that reduce timing errors by 28%. Electronic health records now include timing alerts for high-risk drugs. Some pharmacies offer timed blister packs. The FDA and major EHR vendors like Epic are rolling out tools to support chronotherapy. But community pharmacies and home settings still lag behind-so patient awareness is key.