Why three drugs are still the gold standard after a kidney transplant
If you’ve had a kidney transplant, you’re probably on a mix of three powerful drugs: tacrolimus, mycophenolate, and steroids. This combo isn’t new-it’s been the go-to since the late 1990s. But why? Because no single drug can do the job alone. Together, they block your immune system from attacking the new kidney, while keeping you from falling apart from side effects. It’s a tightrope walk: too little suppression, and your body rejects the organ. Too much, and you’re vulnerable to infections, diabetes, or even cancer.
Back in the day, doctors relied on cyclosporine. But patients on that drug had higher rejection rates-over 20% in the first year. When tacrolimus and mycophenolate came along, rejection dropped to just 8%. That’s not a small win. It’s the difference between keeping your new kidney for 10 years or losing it within five.
Tacrolimus: The immune system’s main brake
Tacrolimus, also known as FK506, is your primary shield against rejection. It works by shutting down T-cells-the immune system’s soldiers that recognize your new kidney as foreign. You take it twice a day, usually in the morning and evening. It hits your bloodstream fast-peak levels within 1.5 to 3 hours-and you start feeling its effect within a day or two.
But here’s the catch: tacrolimus has a razor-thin safety zone. Too little, and rejection kicks in. Too much, and you risk kidney damage, tremors, headaches, or even seizures. That’s why your blood levels are checked constantly. In the first year after transplant, doctors aim for a trough level between 5 and 10 ng/mL. After that, it often drops to 3-7 ng/mL to reduce long-term toxicity.
One of the biggest downsides? It can trigger new-onset diabetes after transplant. About 1 in 5 people develop it. That’s why your blood sugar gets monitored weekly at first. You might also notice high cholesterol, high blood pressure, or tingling in your hands and feet. These aren’t rare-they’re expected. But they’re manageable with diet, exercise, and sometimes extra meds.
Mycophenolate: The silent protector
Mycophenolate (often sold as MMF or CellCept) doesn’t work like tacrolimus. Instead of targeting T-cells directly, it starves the immune system of the building blocks it needs to multiply. Think of it like cutting off the army’s supply lines. It’s especially good at stopping the cells that cause chronic damage over time.
You’ll typically start with 1 gram twice a day-so two pills in the morning, two at night. But many people can’t stick with that dose. Around 25% get severe diarrhea. Another 15-20% develop low white blood cell counts, making them prone to infections. That’s why doctors often lower the dose to 500 mg twice a day, or even stop it altogether if side effects are too rough.
Here’s something most patients don’t know: taking mycophenolate with a proton pump inhibitor (like omeprazole) can make it less effective. If you’re on heartburn meds, tell your transplant team. Also, don’t take it with food-it reduces absorption. Best to take it one hour before or two hours after meals.
And yes, it’s expensive. But it’s worth it. Studies show patients who stay on mycophenolate for at least six months have better long-term kidney survival than those who quit early. It’s not just about avoiding rejection-it’s about protecting your graft for decades.
Steroids: The quick fix with long-term costs
Steroids-usually methylprednisolone or prednisone-are the emergency brake. Right after surgery, you get a 1000-mg IV dose in the operating room. That’s a massive hit designed to calm the immune system’s immediate reaction. Then, the taper begins.
By week 3 or 4, you’re down to 15 mg a day. By 2-3 months, it’s 10 mg. Some centers try to drop to 5 mg or even zero by six months. But here’s the truth: most patients stay on at least 5 mg long-term. Why? Because stopping too fast can trigger late rejection-even years after transplant.
The side effects? They’re real. Weight gain, especially around the face and belly. Acne. Thinning skin that bruises easily. Mood swings. Insomnia. And for women, unwanted facial hair. These aren’t just cosmetic-they affect self-esteem, relationships, and mental health.
That’s why so many centers now test steroid-free regimens. One big 2005 study showed that using a drug called daclizumab (an induction agent) instead of steroids gave the same rejection rates. Eighty-nine percent of patients stayed off steroids at six months. But here’s the catch: induction drugs cost thousands more. And not all patients are eligible. If you’re older, have diabetes, or had a deceased donor kidney, steroids might still be your safest bet.
How the three work together
This isn’t a random cocktail. It’s a layered defense. Tacrolimus stops T-cells from activating. Mycophenolate stops them from multiplying. Steroids put out the fire before it even starts. Together, they cover more ground than any two drugs can.
That’s why the triple combo slashes rejection rates by more than half compared to just tacrolimus and steroids. In one study, rejection dropped from 21% to 8.2%. That’s a 61% improvement. No other combination comes close.
But timing matters. You’re told to space tacrolimus and mycophenolate 2-4 hours apart. Why? Because they compete for the same liver enzymes. Taking them together can make one less effective. And if you miss a dose? Don’t double up. Call your clinic. A single missed dose can tip the balance.
The hidden challenges: Infections, cancer, and long-term damage
Every year, about 1 in 4 adults who get a kidney transplant lose the graft. Why? Not because of rejection. Because of long-term damage. The drugs that save your kidney also slowly wear it down. Tacrolimus causes scarring in the tiny filtering units. Mycophenolate can’t stop that. Steroids speed up bone loss and high blood pressure.
You’re also at higher risk for infections. CMV (cytomegalovirus) is the big one. It can cause fever, fatigue, and even organ damage. Most centers give antiviral meds for the first 3-6 months. Skin cancers? Three to five times more common than in the general population. That’s why you need a full-body skin check every year.
And yes, the risk of lymphoma and other cancers is higher. That’s why the FDA puts black box warnings on all these drugs. But here’s the thing: the risk of dying from rejection without these drugs is far greater than the risk of cancer from them. It’s a trade-off. And it’s one you make every day.
What’s changing? The future of transplant meds
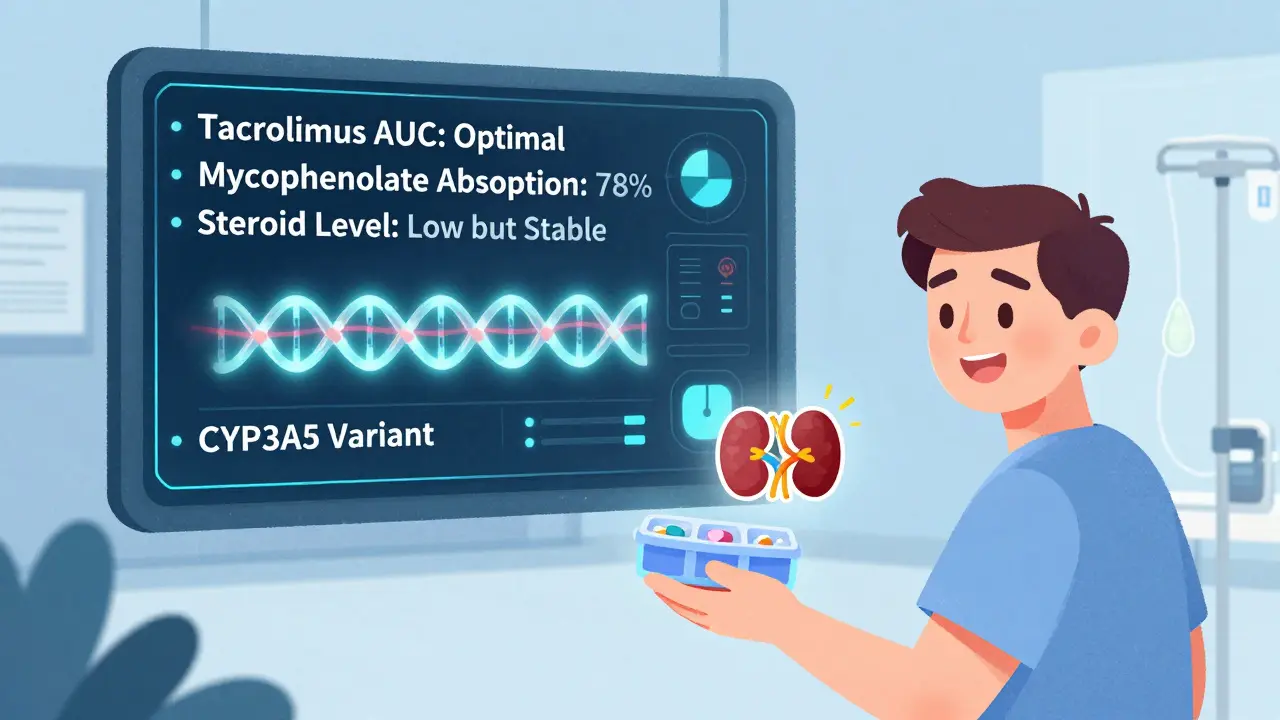
The days of one-size-fits-all immunosuppression are ending. Doctors now know that people metabolize these drugs differently. Some clear tacrolimus fast. Others hold onto it like glue. That’s why monitoring the area under the curve (AUC)-how much drug is in your blood over time-is replacing simple blood level checks. It’s more accurate. And it’s becoming standard in top centers.
Some hospitals are testing gene tests to predict how you’ll handle these drugs. If you have a certain variant in the CYP3A5 gene, you might need twice the dose of tacrolimus. Others are looking at blood biomarkers to tell when you’re over-immunosuppressed. That could mean fewer infections and less cancer down the road.
And steroid-free protocols? They’re growing. More patients are getting induction drugs like basiliximab or alemtuzumab to replace steroids. But they’re not for everyone. If you’re young, healthy, and got a living donor kidney? You might be a candidate. If you’re older or had complications? Steroids might still be your best shot.
One thing’s clear: the future isn’t about removing drugs. It’s about personalizing them. Tailoring doses. Timing them. Monitoring them. That’s where the real progress is.
What patients actually experience
Real people on this regimen don’t talk about pharmacokinetics. They talk about fatigue. About needing to nap after lunch. About avoiding crowds during flu season. About the constant worry: Did I take my pill? Did I eat with my mycophenolate? Is that rash an infection or a side effect?
One patient I spoke with-58, living donor transplant, 7 years out-said the worst part wasn’t the pills. It was the guilt. “I feel like I’m cheating death. Every time I get sick, I wonder if it’s because I skipped a dose.”
Another said she stopped mycophenolate because of diarrhea. Three months later, her creatinine rose. She had to restart it. “I’d rather have the stomach cramps than go back on dialysis.”
These aren’t side effects. They’re the price of survival.
What you need to remember
- Tacrolimus levels must be monitored-don’t skip blood tests.
- Mycophenolate works best on an empty stomach. Take it 1 hour before or 2 hours after meals.
- Steroids are a double-edged sword. Don’t stop them without talking to your team.
- Drug interactions matter. Tell every doctor you see-you’re on immunosuppressants.
- Report any fever, cough, rash, or unusual fatigue. It could be infection, not just a cold.
- Stay up to date on vaccines (flu, pneumonia, COVID). Avoid live vaccines.
- Get annual skin checks. Protect your skin from the sun.
- Don’t stop any drug, even if you feel fine. Rejection can happen silently.
Can I stop taking steroids after a kidney transplant?
Some patients can, but it’s not for everyone. Steroid-free regimens work well in younger, low-risk patients who get induction therapy. But for most-especially those with deceased donor kidneys or prior rejection history-staying on a low dose (5 mg or less) long-term reduces the risk of late rejection. Never stop steroids on your own. Always work with your transplant team.
Why is my mycophenolate dose being lowered?
The most common reasons are gastrointestinal side effects like diarrhea or nausea, or low white blood cell counts (leukopenia). About 20-30% of patients need a dose reduction. Lowering it to 500 mg twice daily often helps while still protecting your kidney. Stopping it completely increases rejection risk, so dose reduction is preferred over discontinuation.
What happens if I miss a dose of tacrolimus?
Missing one dose rarely causes immediate rejection, but it increases your risk. If you miss a dose, take it as soon as you remember-unless it’s close to your next dose. Never double up. Call your transplant center for advice. Consistency matters more than perfection. Set phone alarms. Use pill organizers. This is non-negotiable.
Do these drugs cause weight gain?
Steroids are the main culprit-they increase appetite and cause fluid retention. Tacrolimus and mycophenolate don’t directly cause weight gain, but fatigue from all three can make you less active. Managing weight requires diet, exercise, and sometimes insulin if you develop diabetes. Talk to a dietitian who specializes in transplant care.
How long will I need to take these drugs?
For life. Even if your kidney is working perfectly after 10 or 20 years, stopping immunosuppression will cause rejection. There’s no cure for transplant rejection-only prevention. That’s why these drugs are lifelong. But the doses may change. Some people reduce steroids after 6 months. Others switch to lower-toxicity alternatives. But you’ll always need at least one immunosuppressant.
Final thoughts: Survival isn’t just about the transplant
The day you get your new kidney is a miracle. But the real work starts after you leave the hospital. These three drugs keep you alive. But they also change your body, your routine, your mindset. You’re not just managing a disease-you’re managing a new way of living.
There’s no perfect regimen. No drug without risk. But the triple therapy of tacrolimus, mycophenolate, and steroids remains the most proven path to long-term survival. The future will bring better tools-personalized dosing, biomarkers, smarter monitoring. But for now, sticking to your plan, knowing your numbers, and staying in touch with your team is the best thing you can do.
Your kidney isn’t just an organ. It’s a gift. And these drugs? They’re the price you pay to keep it alive.
Donna Macaranas
February 1, 2026 AT 18:51Still grateful every morning.
Jaden Green
February 2, 2026 AT 00:42Angel Fitzpatrick
February 3, 2026 AT 14:06Nidhi Rajpara
February 4, 2026 AT 09:50Chris & Kara Cutler
February 5, 2026 AT 21:54Rachel Liew
February 7, 2026 AT 12:49Nicki Aries
February 7, 2026 AT 20:29Melissa Melville
February 8, 2026 AT 04:33Well, I guess that’s why they call it a transplant and not a ‘free lunch.’ 😅
Bryan Coleman
February 9, 2026 AT 17:46Sami Sahil
February 10, 2026 AT 20:52franklin hillary
February 12, 2026 AT 10:16Bob Cohen
February 14, 2026 AT 01:34Ishmael brown
February 15, 2026 AT 22:45Aditya Gupta
February 16, 2026 AT 02:10