Thiazide & Vitamin D Risk Calculator
Calcium Risk Assessment
This calculator estimates your risk of hypercalcemia when taking thiazide diuretics with vitamin D supplements based on medical research.
Estimated Calcium Level: mg/dL
Risk Level:
When you're taking a thiazide diuretic like hydrochlorothiazide for high blood pressure, and you're also popping a vitamin D supplement for bone health, you might think you're doing everything right. But there's a quiet, dangerous interaction happening inside your body-one that can push your calcium levels into dangerous territory without you even noticing.
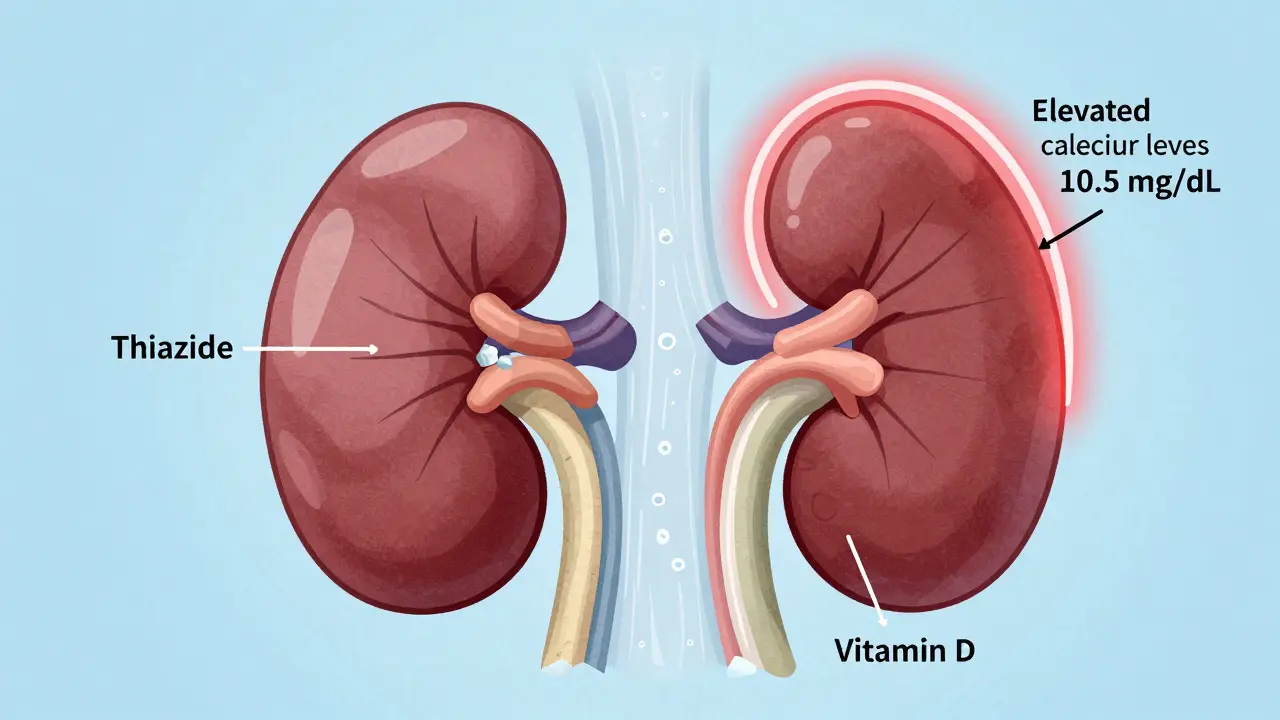
How Thiazide Diuretics Change Your Calcium Balance
Thiazide diuretics-drugs like hydrochlorothiazide (Microzide), chlorthalidone, and indapamide-are commonly prescribed for hypertension. They work by blocking sodium reabsorption in the kidney’s distal convoluted tubule. But here’s the twist: while they help flush out sodium and water, they also cause your kidneys to hold onto calcium instead of letting it leave in your urine. Studies show this reduces urinary calcium excretion by 30-40%. That sounds helpful, right? But when combined with extra vitamin D, it becomes a problem.Normally, your body keeps calcium in a tight balance. Your bones store it, your intestines absorb it from food, and your kidneys decide how much to keep or dump. Thiazides mess with the kidney part-making it harder for calcium to escape. That’s fine if your diet and supplement intake are normal. But when you add high-dose vitamin D, you’re turning up the volume on calcium absorption from your gut.
Why Vitamin D Makes Things Worse
Vitamin D isn’t just a vitamin. In its active form, calcitriol, it acts like a hormone that tells your intestines to absorb more calcium from food. A 2020 meta-analysis found that vitamin D can boost intestinal calcium absorption by 30% to 80%, depending on the dose. So if you’re taking 5,000 IU or more daily-a common dose found in over-the-counter supplements-you’re essentially flooding your system with calcium.Now imagine this: your kidneys are holding onto more calcium because of the thiazide, and your gut is pulling in way more calcium because of the vitamin D. That’s a double hit. Your blood calcium rises. And when serum calcium climbs above 10.5 mg/dL, you’ve crossed into hypercalcemia territory.
The Numbers Don’t Lie
This isn’t theoretical. A 2021 study from the Mayo Clinic found that patients on long-term thiazide therapy had an 8-12% risk of hypercalcemia if they took more than 4,000 IU of vitamin D daily. Compare that to just 2-3% risk in those taking thiazides alone. The American Heart Association says 15% of emergency visits for drug-induced hypercalcemia involve this exact combo.And it’s not just big doses. One nurse practitioner on Reddit reported three hospitalizations in six months from patients taking 5,000 IU of vitamin D3 with hydrochlorothiazide. Their calcium levels hit over 11 mg/dL-well above the safe limit. Symptoms? Fatigue, constipation, nausea, confusion, frequent urination. Many patients dismiss these as "just getting older" or "side effects of meds." But they’re warning signs.
Who’s Most at Risk?
Older adults are the most vulnerable. About 80% of people over 65 take either a thiazide diuretic or vitamin D supplement. Many take both. A 2022 National Council on Aging survey found 61% of seniors on thiazides didn’t know they needed to check their calcium levels when taking vitamin D. That’s a massive gap in awareness.People with pre-existing kidney issues, parathyroid disorders, or borderline high calcium (above 10.2 mg/dL) are at even higher risk. The American Geriatrics Society Beers Criteria specifically lists this combination as potentially inappropriate for older adults with elevated calcium. Yet, it’s still widely prescribed.
What About Other Diuretics?
Not all diuretics are the same. Loop diuretics like furosemide actually make you pee out more calcium-so they don’t raise the risk. Potassium-sparing diuretics like spironolactone have little to no effect on calcium. If you’re on a thiazide and need vitamin D, your doctor might consider switching you to one of these alternatives.Chlorthalidone, a longer-acting thiazide, has an even stronger calcium-sparing effect than hydrochlorothiazide-up to 42% reduction in urinary calcium. So if you’re on chlorthalidone, the risk is higher. But even hydrochlorothiazide at 25 mg daily can be enough to trigger problems when paired with high-dose vitamin D.
How to Stay Safe
The good news? This risk is totally manageable-if you know what to do.- Get your serum calcium checked before starting vitamin D if you’re on a thiazide. Then retest at 3 months, and every 6-12 months after that.
- Keep vitamin D at 800-1,000 IU daily. That’s enough for bone health and immune support without pushing calcium too high. Avoid doses above 2,000 IU unless specifically monitored by a doctor.
- Use the lowest effective thiazide dose. Hydrochlorothiazide 12.5 mg works just as well for blood pressure as 25 mg for many people-and carries less calcium risk.
- Ask about alternatives. If you’re at high risk, ask your doctor if a different blood pressure med (like an ACE inhibitor or calcium channel blocker) could replace the thiazide.
- Don’t self-prescribe vitamin D. Many people take 5,000 IU because they read it’s "better" or "more effective." That’s not true for everyone. More isn’t always better.

What Clinicians Are Doing About It
Some health systems are stepping up. Kaiser Permanente now uses electronic health record alerts that pop up when a patient is prescribed a thiazide and a vitamin D dose over 2,000 IU. Since implementing this, they cut unsafe combinations by 63%.Pharmacist-led interventions have also proven effective. A 2022 study showed that when pharmacists proactively checked calcium levels and adjusted doses, hypercalcemia dropped from 11.3% to just 2.7% in a group of 450 patients.
But awareness is still low. Only 42% of internists know how often to check calcium in these patients. Most still think annual testing is enough. It’s not. Every 6 months is the standard for those on this combo.
The Bigger Picture
The vitamin D supplement market is worth nearly $2 billion. Thiazide prescriptions in the U.S. hit 53.7 million in 2022. Millions of people are on both. That’s not a coincidence-it’s a public health blind spot.There’s new research too. A 2023 FDA-approved test called CalcCheck looks at genetic variants in the calcium-sensing receptor to predict who’s most likely to develop hypercalcemia on this combo. It’s not widely available yet, but it’s a step toward personalized safety.
And while some experts argue the risk is overstated, the evidence is mounting. The 2024 American Heart Association guidelines are expected to tighten recommendations further. Waiting for guidelines to change isn’t a strategy. Monitoring your calcium is.
Bottom Line
You don’t need to stop vitamin D. You don’t need to stop your blood pressure pill. But you do need to know how they work together-and how to keep your calcium in check.If you’re on a thiazide diuretic and taking vitamin D:
- Keep your dose at 800-1,000 IU daily.
- Get your blood calcium tested every 6 months.
- Watch for symptoms: fatigue, constipation, frequent urination, confusion.
- Ask your doctor if a different blood pressure medication might be safer.
This interaction is preventable. It’s not rare. And it’s not something you should ignore.
Chris Cantey
January 5, 2026 AT 20:36Been on HCTZ for 12 years. Took 5,000 IU of D3 because my doctor said "it’s safe." Last year my calcium hit 11.4. ER visit. They didn’t connect the dots until I mentioned the supplement. Now I’m down to 1,000 IU. No symptoms. No drama. Just quiet survival.
Don’t assume "natural" means harmless.
Abhishek Mondal
January 7, 2026 AT 18:51Let’s be precise: the mechanism isn’t "double hit"-it’s a pharmacokinetic synergy between VDR upregulation and NCC inhibition. The Mayo Clinic study had a selection bias: they excluded patients on calcium channel blockers, which skews the risk profile. Also, 4,000 IU is the UL-not a threshold for toxicity. The FDA’s RDA for adults is 600 IU; the fact that people treat supplements like vitamins rather than hormones is the real problem.
And yes, I’ve reviewed the 2023 CalcCheck paper. It’s promising-but still not in the DSM-5-TR. So, no, I won’t stop my 5,000 IU until you prove it’s not a Big Pharma smear campaign.
Terri Gladden
January 8, 2026 AT 01:54OMG I JUST REALIZED I’M TAKING BOTH!! I’VE BEEN FEELING SO WEIRD LATELY-CONSTIPATED, TIRED, LIKE MY BRAIN IS IN SLOW MOTION!! I THOUGHT IT WAS JUST AGING OR STRESS!! I JUST DELETED MY VITAMIN D ORDER ON AMAZON!! I HOPE I DIDN’T DAMAGE MY KIDNEYS!!
Jennifer Glass
January 9, 2026 AT 00:17This is one of those posts that feels like it was written for someone like me-someone who’s been told "take vitamin D for immunity" and "take HCTZ for blood pressure" without ever being told how they interact.
It’s not just about the numbers-it’s about how little we’re taught to think about medication interactions as patients. We’re handed prescriptions and supplements like candy, then expected to just "trust the system."
I got my calcium checked last month after reading this. It was 10.1. My doctor said "it’s fine," but I’m still getting it rechecked in three months. Better safe than sorry.
And yeah, I dropped my D3 from 2,000 to 1,000 IU. No regrets. My bones aren’t going anywhere, and my kidneys are already working hard enough.
Joseph Snow
January 9, 2026 AT 20:25Let’s not pretend this isn’t a controlled narrative. The AHA, Kaiser, and "pharmacist-led interventions" are all funded by the same entities that profit from lab testing and alternative antihypertensives. Vitamin D is one of the cheapest, most studied supplements on the planet. The hypercalcemia risk is exaggerated to push people toward more expensive drugs. Why else would they push a $500 genetic test? The real danger here is losing autonomy to medical gatekeepers who profit from fear.
My calcium is 9.8. I take 5,000 IU daily. I’ve never had a symptom. The system wants you afraid. Don’t be.
en Max
January 11, 2026 AT 09:30Thank you for this meticulously referenced, clinically grounded exposition. The integration of epidemiological data (Mayo Clinic, 2021), pharmacodynamic principles (NCC inhibition → reduced calciuresis), and public health metrics (Kaiser’s EHR intervention) constitutes a paradigmatic case study in translational medicine.
It is imperative that clinicians recognize that vitamin D, in pharmacologic doses, functions not as a micronutrient, but as a hormonal modulator-with downstream effects on renal tubular reabsorption, intestinal calcium transport, and parathyroid feedback loops.
Moreover, the 61% awareness gap among seniors underscores a systemic failure in patient education. Proactive, structured counseling-ideally delivered via pharmacy-based medication therapy management programs-is not merely advisable; it is ethically obligatory.
Finally, the 63% reduction in unsafe combinations post-intervention is not a statistic-it is a moral victory.
Let us not underestimate the power of vigilance, nor overestimate the safety of self-prescribed supplementation.
Angie Rehe
January 11, 2026 AT 22:10Oh please. You’re telling me I can’t take my 5,000 IU because I’m on a water pill? My doctor said it’s fine. My blood pressure is perfect. My bones are strong. I’m 72 and I hike every weekend. You think I’m going to stop because some Reddit post says so? You’re scaring people into giving up what’s keeping them healthy so you can sell them more tests and more expensive meds. I’ve had my calcium checked-twice. It’s fine. Stop gaslighting seniors.
And don’t even get me started on the "calcium-sensing receptor" test. That’s just another $$$ scam.
Jacob Milano
January 13, 2026 AT 17:17Man, this hit different. I’ve been on hydrochlorothiazide since my 50s, and I’ve been taking D3 like it’s candy since the pandemic. I thought I was being proactive. Turns out I was just being reckless.
But here’s the thing-I’m not mad. I’m grateful. This post didn’t scare me; it woke me up. I called my doctor this morning. We dropped my D3 to 1,000 IU and scheduled a calcium panel next week. No drama. No panic. Just quiet, smart adjustments.
And hey-if you’re reading this and you’re on the same combo? Don’t freak out. Just check. Just ask. Just breathe. You’re not broken. You’re just human. And humans need good info, not guilt.
Thanks for writing this. Seriously. You saved someone today.