Herbal teas might seem harmless, but they can mess with your meds in ways you never expected.
You drink chamomile tea to unwind. Green tea for a gentle energy boost. Hibiscus tea because it’s tart and feels like a treat. But if you’re on blood thinners, blood pressure meds, antidepressants, or heart drugs, what you sip could be working against you-sometimes dangerously.
Unlike prescription drugs, herbal teas aren’t tested for safety before they hit store shelves. The FDA treats them like food, not medicine. That means no one checks if mixing your evening cup of St. John’s wort tea with your antidepressant could make you feel worse-or worse, stop your medication from working at all.
Here’s the hard truth: herbal teas can change how your body handles medications. They can make drugs stronger, weaker, or cause side effects you didn’t sign up for. And most people have no idea.
Green tea isn’t just a health drink-it’s a drug interceptor
Green tea gets a lot of praise for antioxidants. But that same compound, epigallocatechin gallate (EGCG), is also a silent saboteur when it comes to medications.
Studies show green tea can slash the amount of atorvastatin (a common cholesterol drug) in your blood by up to 39%. That means your statin stops working. Your cholesterol climbs. You think you’re doing everything right-diet, exercise, meds-and yet your numbers are still high. The culprit? Your morning tea.
Even worse, green tea can reduce nadolol (a beta-blocker for heart rhythm and blood pressure) by 85%. That’s not a typo. One study with just 12 people showed a near-total drop in drug levels after drinking three strong cups daily. For someone relying on that drug to prevent a heart attack, that’s life-threatening.
It’s not just about the tea leaves. Green tea extract in pills or capsules is even more dangerous. But even brewed tea, if strong and consumed daily, can interfere. The reason? It blocks transporters in your gut and liver that move drugs into your bloodstream. It also slows down how fast your body breaks down certain meds.
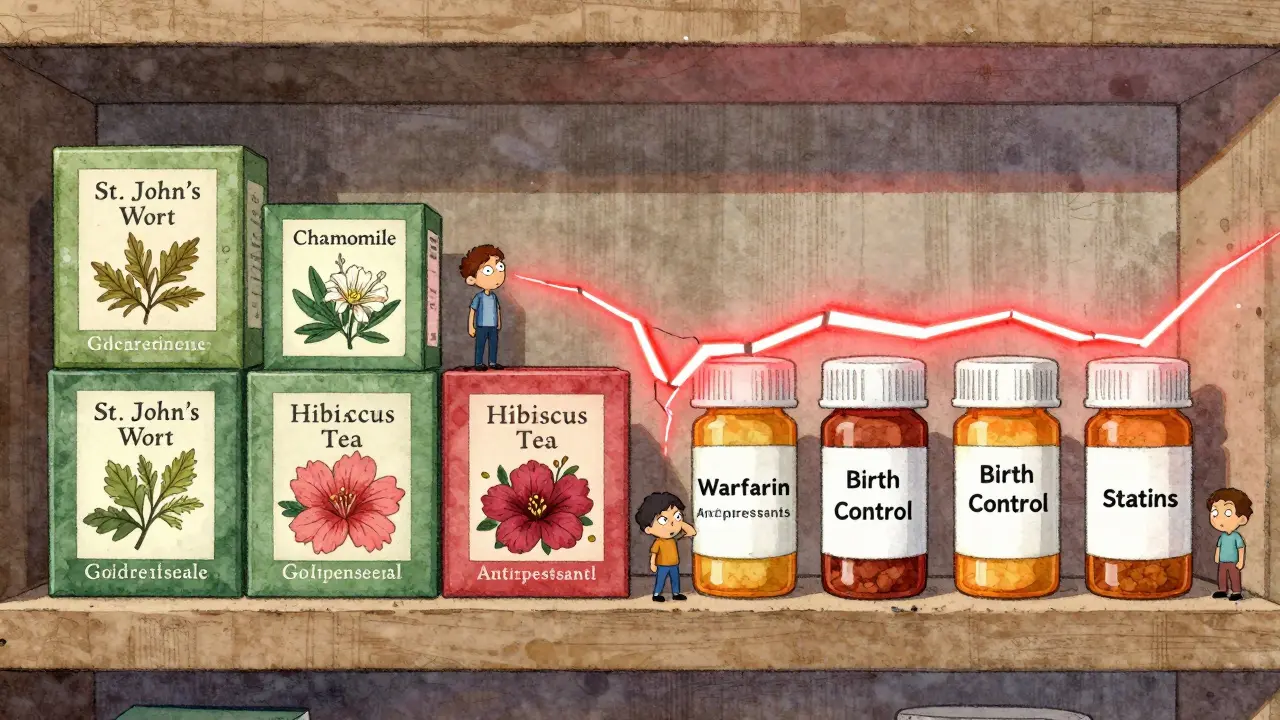
Chamomile, hibiscus, and goldenseal: quiet troublemakers
Chamomile tea is calming. But if you’re on birth control pills, it might be making them useless. Early research suggests chamomile’s apigenin interferes with liver enzymes that process hormones. One missed pill is bad. Daily tea interference? That’s a whole different risk.
Hibiscus tea lowers blood pressure. That sounds good-until you’re already on lisinopril or losartan. Combine them, and your blood pressure can crash below 90 mmHg. Dizziness. Fainting. Falls. Emergency room visits. It’s happened. People thought they were being healthy. They weren’t.
Goldenseal, often brewed as a tea for colds or digestion, is a major red flag. It shuts down two key liver enzymes-CYP2D6 and CYP3A4-that process more than half of all prescription drugs. That includes antidepressants, painkillers, statins, and even some cancer drugs. One study found it can reduce the effectiveness of codeine by 40%. That means your pain doesn’t go away. And you might end up taking more, thinking it’s not working.
Herbs that thin blood: a silent combo
If you’re on warfarin (Coumadin), rivaroxaban, or apixaban, your doctor monitors your blood clotting closely. Now add ginkgo biloba, ginger, garlic, or chamomile tea to the mix.
These herbs act like aspirin-they make platelets less sticky. That’s fine on its own. But with blood thinners? You’re stacking the deck. The result? Easy bruising, nosebleeds, blood in urine, or worse-internal bleeding. The Mayo Clinic documented cases of people on warfarin who started drinking ginkgo tea and ended up in the ER with a brain bleed.
Even cranberry juice, often thought of as safe, has been linked to spikes in INR (a blood clotting measure) in some people on warfarin. Other people? No effect. That inconsistency is part of the problem. You can’t predict who it’ll hit. So the safest move? Avoid it altogether if you’re on anticoagulants.
St. John’s wort: the hidden mood killer
St. John’s wort is one of the most dangerous herbal teas for people on antidepressants, birth control, or HIV meds. It doesn’t just interfere-it actively speeds up how fast your body gets rid of these drugs.
Take SSRIs like sertraline or fluoxetine. Add St. John’s wort tea, and your brain gets less of the drug. Depression comes back. Anxiety spikes. You think your meds stopped working. They didn’t. Your tea did.
Same goes for birth control. Women have gotten pregnant while on the pill and drinking St. John’s wort daily. Not because they missed a pill. Because the tea made the pill ineffective.
The National Center for Complementary and Integrative Health calls this one of the most well-documented herb-drug interactions. And yet, people still buy it labeled as “natural mood support.”

Who’s most at risk? (Spoiler: it’s more people than you think)
You might think this only affects elderly folks on 10 pills a day. But it’s not that simple.
People over 65 are the most likely to use herbal teas and meds at the same time. But younger adults? They’re catching up fast. Functional teas-blends marketed for sleep, immunity, or stress-are everywhere. You can buy them at the grocery store, next to the coffee.
And here’s the kicker: most people don’t tell their doctors about them. A 2022 Mayo Clinic review found that only 25% of older adults who use herbal supplements mention them to their providers. Why? They don’t think tea counts as a supplement. Or they assume it’s harmless. Or they’re afraid their doctor will judge them.
That silence is deadly. Doctors can’t protect you if they don’t know what you’re taking.
What to do right now
You don’t need to quit herbal tea forever. But you need to be smart.
- Make a list. Write down every tea you drink daily. Include blends. Include occasional ones. Write the name, how often, and how strong.
- Bring it to your next appointment. Don’t say, “I drink chamomile.” Say, “I drink two cups of Yogi Tea Sleepytime every night.” Be specific.
- Ask: ‘Could this tea affect my meds?’ Don’t assume your doctor knows. Ask directly about each tea you drink.
- Avoid concentrated extracts. Tea is usually safe. Capsules, tinctures, or powders? High risk. Skip them if you’re on meds.
- Watch for warning signs. Unexplained bruising, dizziness, sudden mood changes, or meds that suddenly don’t work? Stop the tea and call your doctor.
The FDA says it plainly: “Natural doesn’t mean safe.” That’s not marketing. That’s science.
When in doubt, pause
There are no hard-and-fast rules for every tea and every drug. Research is still catching up. But for drugs with a narrow therapeutic index-warfarin, digoxin, cyclosporine, theophylline, lithium-play it safe.
These drugs have a tiny window between helping and harming. Even a small change in how your body handles them can cause serious harm. If you’re on one of these, avoid green tea, St. John’s wort, hibiscus, and goldenseal teas altogether.
For everything else? Talk to your pharmacist. They’re trained to spot these interactions. They see this every day.
Herbal teas aren’t the enemy. But pretending they’re harmless while you’re on prescription meds? That’s the real risk.
Matt W
February 3, 2026 AT 19:05Bridget Molokomme
February 4, 2026 AT 16:30George Firican
February 5, 2026 AT 15:28Vatsal Srivastava
February 6, 2026 AT 17:04Brittany Marioni
February 7, 2026 AT 02:15Monica Slypig
February 8, 2026 AT 15:52Becky M.
February 10, 2026 AT 08:06jay patel
February 10, 2026 AT 19:27Ansley Mayson
February 10, 2026 AT 23:02phara don
February 12, 2026 AT 01:40Hannah Gliane
February 13, 2026 AT 00:38Murarikar Satishwar
February 13, 2026 AT 17:55Dan Pearson
February 13, 2026 AT 19:13