Methotrexate-NSAID Risk Assessment Tool
Assess Your Risk
This tool estimates your risk of kidney injury and methotrexate toxicity when taking NSAIDs with methotrexate, based on the latest medical guidelines.
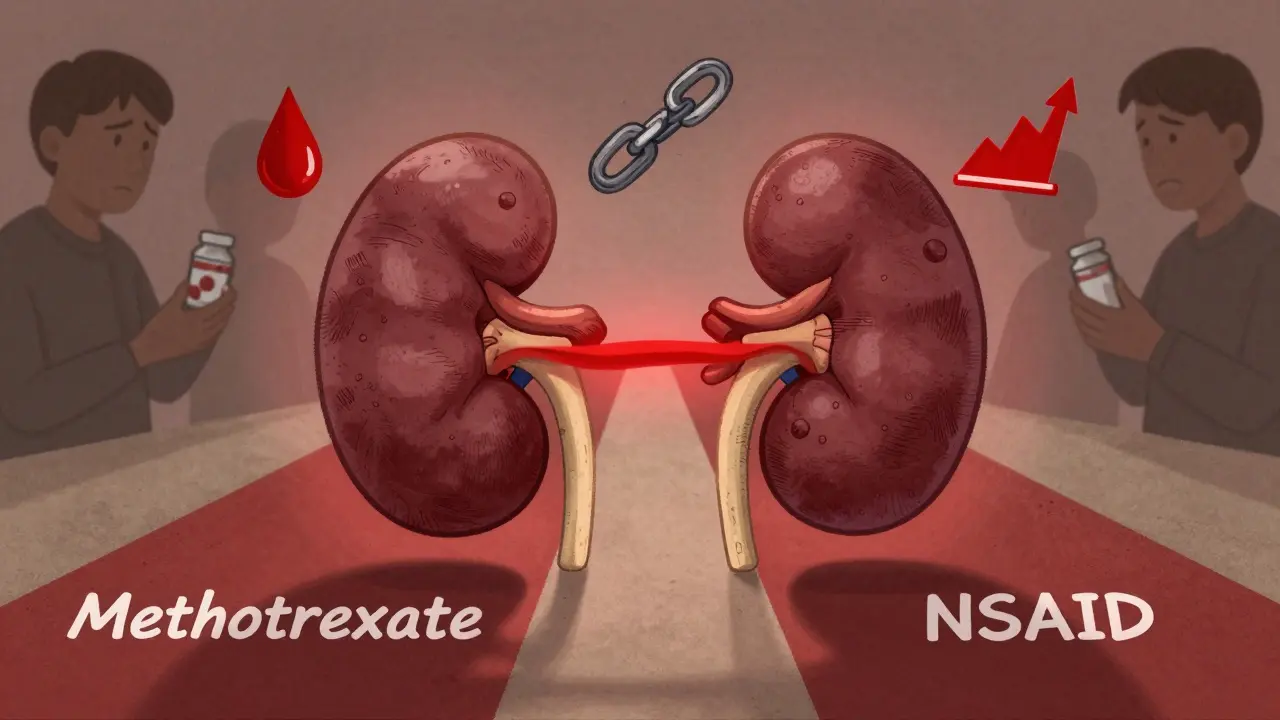
When you're managing rheumatoid arthritis with methotrexate, adding an NSAID for joint pain seems logical. But what if that simple combo could push your kidneys to the edge-or worse? This isn’t theoretical. It’s happening in clinics every day, and many patients don’t even know it’s a risk.
Why Methotrexate and NSAIDs Don’t Mix Well
Methotrexate is cleared almost entirely by your kidneys. At low doses (5-25 mg weekly), it’s used for autoimmune diseases like RA. At high doses (over 150 mg), it’s used for cancer. Either way, your kidneys have to work hard to get it out of your system. That’s where NSAIDs come in-and why they’re dangerous together. NSAIDs like ibuprofen, naproxen, and diclofenac block prostaglandins, chemicals your kidneys use to keep blood flowing. Less blood flow means less methotrexate gets filtered out. Studies show this cuts methotrexate clearance by 25-40%. That’s not a small drop. It’s enough to cause toxic buildup. Worse, NSAIDs can also compete with methotrexate for the same transporters in kidney tubules. This isn’t just reduced flow-it’s direct interference. Some studies show free methotrexate levels rise by up to 30% because NSAIDs push it off proteins in the blood, leaving more active drug floating around.High-Dose vs. Low-Dose: The Risk Difference
Not all methotrexate use is the same. High-dose therapy (usually over 500 mg/m² for cancer) is far more dangerous when mixed with NSAIDs. A 2022 meta-analysis found the risk of life-threatening toxicity-like bone marrow failure or acute kidney injury-jumps 4.7 times. There are documented cases of death. For low-dose methotrexate (the kind most RA patients take), the data is messier. One large 2019 study of over 4,000 RA patients found no major increase in side effects when NSAIDs were added-but only if kidney function was normal. That’s the key. If your eGFR (a measure of kidney function) is below 60 mL/min/1.73m², your risk spikes 3.2 times. A 2021 study showed these patients had a 3.5-fold higher chance of needing hospitalization for kidney injury. It’s not about whether you take an NSAID. It’s about who you are and how well your kidneys are working.Which NSAIDs Are Riskiest?
Not all NSAIDs are created equal. Ketorolac is the worst offender. It cuts methotrexate clearance more than any other NSAID-up to 50% in some cases. That’s why it’s banned in many hospitals for patients on methotrexate. Ibuprofen and naproxen are moderate risk, increasing methotrexate levels by 25-30%. Diclofenac isn’t much better. Celecoxib, a COX-2 inhibitor, is the safest option here. It only raises methotrexate levels by 10-15%. That’s why some rheumatologists will choose celecoxib over ibuprofen if an NSAID is absolutely necessary. But even celecoxib isn’t risk-free. If your kidneys are already struggling, any NSAID can tip you over.What Happens When Toxicity Strikes
Methotrexate toxicity doesn’t always come with warning signs. Many patients feel fine until their blood work shows disaster. Serum creatinine rises. White blood cell counts crash. Liver enzymes spike. Mouth sores appear. Fatigue hits like a wall. In severe cases, patients need leucovorin rescue-a drug that counteracts methotrexate’s effects. Reddit user ‘RAWarrior2020’ described it perfectly: “My rheumatologist prescribed naproxen without checking my kidney function. Three days later, my white blood cell count dropped to 1.8. I spent two weeks on leucovorin.” That’s not rare. FDA data shows 78% of serious cases involved patients who hadn’t had kidney tests in the past 30 days. Routine blood work isn’t optional-it’s lifesaving.
How Doctors Should Handle This
The American College of Rheumatology’s 2022 guidelines are clear:- Avoid NSAIDs entirely if your eGFR is below 60.
- If you must use one, pick the lowest dose for the shortest time.
- Space methotrexate and NSAID doses by at least 12 hours to avoid peak overlap.
- Check creatinine and complete blood count 48-72 hours after starting the NSAID.
What Patients Can Do
You’re not powerless here. If you’re on methotrexate:- Ask your doctor: “What’s my eGFR? Is it above 60?”
- Don’t take over-the-counter NSAIDs without telling your rheumatologist.
- Know your blood test schedule. If they’re not checking your kidneys every 4-6 weeks, ask why.
- Keep a log of any new symptoms: fatigue, nausea, mouth sores, bruising.
Alternatives to NSAIDs
If you need pain relief, there are safer options:- Acetaminophen (up to 3,000 mg/day): No known interaction with methotrexate. First-line for mild pain.
- Low-dose opioids: Only for short-term use, like after surgery. Avoid long-term use due to addiction risk.
- DMARDs: Sometimes, adjusting your RA treatment (like adding sulfasalazine or hydroxychloroquine) reduces inflammation enough to cut pain without NSAIDs.

The Bigger Picture: Monitoring Saves Lives
A 2023 study found pharmacist-led interventions reduced methotrexate-NSAID interactions by 63% in Medicare patients. How? By screening prescriptions, educating patients, and flagging risky combinations before they happen. This isn’t just about one drug combo. It’s about systems. Too many patients get NSAIDs prescribed like aspirin-without thinking. But methotrexate isn’t aspirin. It’s a narrow-therapeutic-index drug. A tiny change in clearance can be deadly. The FDA and EMA both updated labels in 2022-2023 to warn about this. But warnings don’t stop mistakes. Monitoring does.What’s Next? Genetic Testing and Real-Time Monitoring
Emerging research shows genetics play a role. About 15% of Caucasians carry a gene variant (SLC19A1 80G>A) that makes them absorb more methotrexate. When they take NSAIDs, their levels spike 40% higher than others. In the near future, point-of-care devices may let doctors check methotrexate levels in minutes-not days. Clinical trials are already underway. This could change everything. Until then, the rule is simple: Don’t guess. Test.Can I take ibuprofen with methotrexate?
It’s possible, but only if your kidney function is normal (eGFR above 60) and you’re on low-dose methotrexate. Even then, use the lowest dose of ibuprofen for the shortest time possible. Always get your creatinine and blood count checked 48-72 hours after starting it. Never take ibuprofen without your doctor’s approval if you’re on high-dose methotrexate.
What are the signs of methotrexate toxicity?
Symptoms include extreme fatigue, mouth sores, nausea, vomiting, unusual bruising or bleeding, dark urine, and yellowing of the skin or eyes. But often, the first sign is a blood test showing low white blood cells or high creatinine-before you feel anything. That’s why regular lab checks are critical.
Is celecoxib safer than other NSAIDs with methotrexate?
Yes, celecoxib is the safest NSAID option when combined with methotrexate. It increases methotrexate levels by only 10-15%, compared to 25-50% with other NSAIDs. But it’s not risk-free. If your kidneys are impaired, even celecoxib can cause toxicity. Always monitor kidney function and blood counts.
How often should I get blood tests if I’m on methotrexate and an NSAID?
If you’re starting an NSAID while on methotrexate, get a creatinine and complete blood count test 48-72 hours after your first NSAID dose. After that, continue testing every 4-6 weeks if you’re on low-dose methotrexate. For high-dose therapy, methotrexate levels must be checked at 24, 48, and 72 hours post-infusion if NSAIDs are used.
Can I take acetaminophen instead of NSAIDs with methotrexate?
Yes, acetaminophen (up to 3,000 mg per day) is the preferred pain reliever for people on methotrexate. It doesn’t affect kidney function or methotrexate clearance. It’s not as strong for inflammation, but it’s much safer. Talk to your doctor about using it as your first-line option for pain.
Why do some people take NSAIDs with methotrexate and never have problems?
They’re likely the lucky ones-those with healthy kidneys, normal dosing, and regular monitoring. Many patients who have no issues are also getting their labs checked every month. The danger isn’t the combo itself-it’s the lack of monitoring. Without blood tests, toxicity can sneak up silently.
Peter Sharplin
January 25, 2026 AT 05:54Been on methotrexate for 6 years with RA. Took ibuprofen for years without issue-until my eGFR dipped to 58. One naproxen pill and my WBC crashed to 2.1. They put me on leucovorin. Lesson learned: labs aren’t optional. I now use acetaminophen and check my numbers every 4 weeks like clockwork.
Don’t wait for symptoms. By then, it’s too late.
John Wippler
January 26, 2026 AT 00:05It’s wild how we treat methotrexate like it’s just another pill. It’s not. It’s a scalpel in a world of butter knives. NSAIDs? They’re the blindfold you put on before stepping off a cliff. The body doesn’t care about your ‘I’ve been fine for years’ story. It only cares about transporters, creatinine, and glomerular filtration rates.
Every time someone says ‘my doctor said it’s fine,’ I hear a system that’s still asleep. We need pharmacists on the front lines-not just after the crash.
rasna saha
January 27, 2026 AT 20:41Thank you for writing this. I’m from India and my rheumatologist here barely checks labs unless I beg. I started asking for eGFR and CBC every month after reading your post. My doctor was surprised-but then admitted most patients don’t get tested regularly here. This info could save lives in places where meds are easy to get but monitoring isn’t.
Stay safe, everyone.
Skye Kooyman
January 28, 2026 AT 19:15celecoxib ftw
no more ibuprofen for me
shivam utkresth
January 29, 2026 AT 02:21Man, this is the kind of shit that gets lost in translation in global healthcare. In India, we got methotrexate over the counter like aspirin. NSAIDs? Even easier. No labs, no questions, just ‘take two for pain.’
I’ve seen three friends end up in ICU for MTX toxicity. One guy didn’t even know he had RA-he just had ‘bad knees’ and took pills for 3 years.
We need community health workers to explain this, not just doctors in fancy clinics. Knowledge is the real DMARD here.
Kipper Pickens
January 30, 2026 AT 04:53Let’s unpack the pharmacokinetics: methotrexate is primarily excreted via renal tubular secretion via RFC and BCRP transporters. NSAIDs inhibit these via competitive binding and reduce renal perfusion via COX-1 mediated vasoconstriction. The net effect is reduced CLrenal and increased AUC-especially problematic in low-dose regimens where therapeutic index is narrow.
Also, plasma protein binding displacement by NSAIDs increases free MTX fraction, amplifying cytotoxicity. Celecoxib has minimal affinity for these transporters-hence its relative safety profile.
Bottom line: it’s not anecdotal. It’s biochemistry.
Aurelie L.
January 31, 2026 AT 22:04My mom died from this. She was 72. Took naproxen for arthritis. Methotrexate for RA. No blood work for 8 months. They found her in the kitchen, pale as paper. WBC 0.9. She didn’t even know she was at risk.
Why is this not on every prescription bottle?
Joanna Domżalska
January 31, 2026 AT 23:15So let me get this straight. You’re saying if I’m healthy, I can’t take ibuprofen with methotrexate? But I’ve been doing it for 10 years and I run marathons. Maybe the real problem is doctors being scared of lawsuits and scaring patients into acetaminophen.
Also, why do we assume everyone has bad kidneys? Maybe I’m just one of those people who don’t need to be coddled.
James Nicoll
February 1, 2026 AT 10:04So basically, the FDA says ‘don’t mix’ but your doctor says ‘eh, you’ll be fine.’
Meanwhile, the real villain is the $12 bottle of ibuprofen at the corner store that doesn’t come with a 12-page warning pamphlet.
Maybe the solution isn’t more blood tests… maybe it’s making NSAIDs prescription-only when you’re on MTX.
Just saying.
Uche Okoro
February 1, 2026 AT 16:22As a clinical pharmacologist based in Lagos, I can confirm this interaction is grossly underrecognized in LMICs. Methotrexate is often dispensed without renal function screening. NSAIDs are freely available in street pharmacies. The mortality rate from this combo is likely underreported by a factor of 5.
Our hospital started a pharmacist-led MTX safety initiative last year. We reduced adverse events by 71%. It’s not rocket science-it’s logistics. And it’s doable.
Ashley Porter
February 2, 2026 AT 05:08Just got my labs back: eGFR 62, WBC 5.4. Took celecoxib for 3 weeks. No spike. Still, I’m not taking any chances. I’m switching to acetaminophen and scheduling my next blood draw for next week.
Knowledge is power, but consistent monitoring is armor.
Faisal Mohamed
February 2, 2026 AT 14:02Imagine if we could just scan your blood and see MTX levels in real time like a glucose monitor 🤯
That’s the future. Until then, I’m sticking with Tylenol and yoga. 🙏
Also, celecoxib > ibuprofen. No debate. 🧪
Alexandra Enns
February 4, 2026 AT 02:24Canadian here. Our system is way better than the US. We get mandatory labs every 6 weeks with methotrexate. No exceptions. If your doctor doesn’t order them, they get audited. That’s why we don’t have these horror stories here.
Stop romanticizing ‘natural healing.’ This isn’t a lifestyle blog. It’s life-or-death pharmacology.
Marie-Pier D.
February 5, 2026 AT 14:22To everyone reading this: you’re not alone. I was scared to speak up about my MTX side effects. I thought I was being dramatic. Turns out, my fatigue and mouth sores were early signs of toxicity.
Ask for your eGFR. Ask for your CBC. Write it down. Bring it to your next appointment.
You deserve to feel safe in your own body. 💛