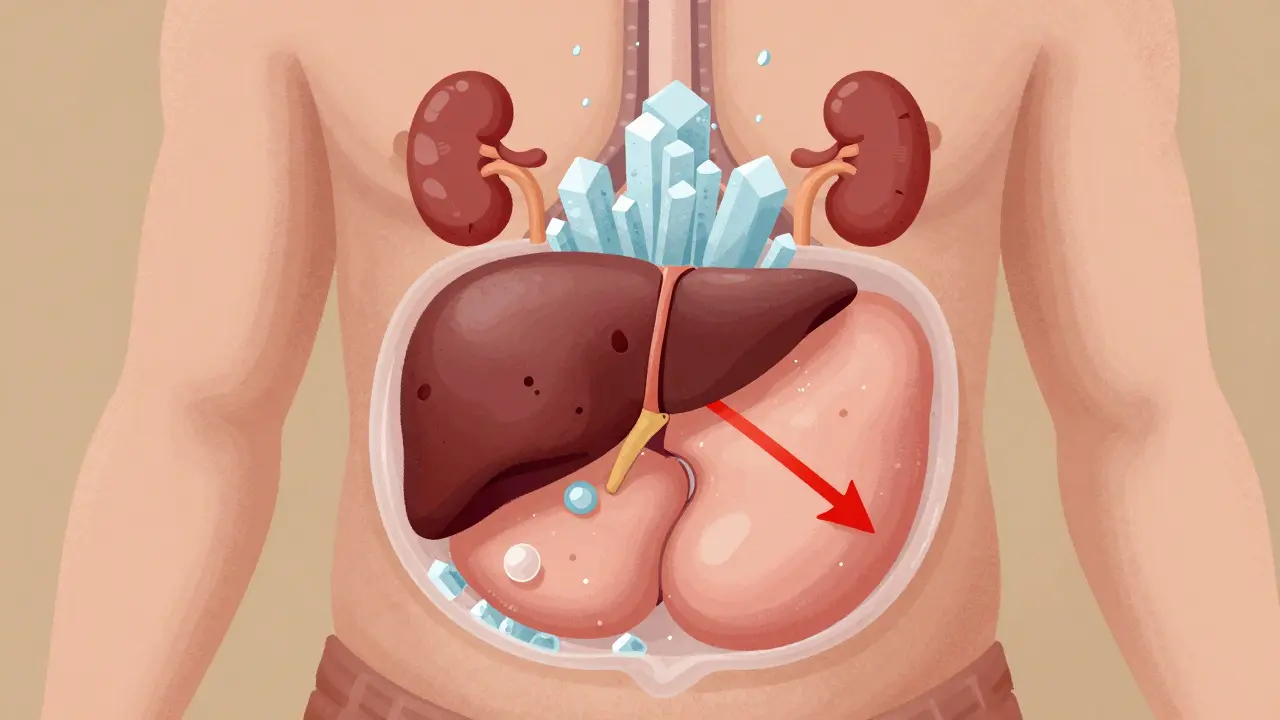
When your liver starts to fail, fluid doesn’t just disappear-it builds up. In the belly. Around the organs. In the legs. This is ascites, and it’s not just uncomfortable. For people with cirrhosis, it’s a warning sign that things are getting serious. About half of all cirrhosis patients will develop ascites within 10 years. And once it shows up, survival drops to about 50% within two years. That’s not a guess-it’s from the American Association for the Study of Liver Diseases (AASLD) 2023 guidelines. The good news? We have tools to fight it. The bad news? The rules aren’t as clear as they used to be.
Why Fluid Builds Up in the Belly
It starts with high pressure in the liver’s blood vessels. When the liver is scarred from cirrhosis, blood can’t flow through easily. Pressure builds. The kidneys sense this as low blood volume-even though there’s too much fluid in the body. So they hold onto salt and water like they’re running out. That’s the core problem: your body thinks it’s dehydrated, so it keeps fluid in. And that fluid ends up pooling in the abdomen. This isn’t just about drinking too much water. It’s about sodium. Too much sodium in, not enough out. That’s the trigger.The Old Rule: Eat Less Than 2 Grams of Sodium a Day
For decades, the standard advice was simple: cut sodium to less than 2 grams per day. That’s about 5 grams of salt-less than a teaspoon. Hospitals, dietitians, and doctors all pushed this. The logic was clear: less sodium = less fluid retention. But here’s the catch: no one ever proved it worked well in real life. Most people with cirrhosis can’t stick to it. A 2021 study found fewer than 40% of patients actually followed the 2-gram limit. Why? Because 75% of the sodium we eat doesn’t come from the salt shaker. It’s in bread, canned soup, deli meats, sauces, even breakfast cereal. Trying to avoid all of it is exhausting. And dangerous. Many patients are already malnourished. Starving them of salt can make that worse.The New Debate: Is Less Sodium Even Better?
Recent studies are turning the old advice upside down. Two randomized trials published between 2017 and 2022 found that patients who ate 5 to 6.5 grams of sodium a day-roughly what most people normally eat-did better than those on strict restriction. They had less ascites. They needed fewer procedures to drain fluid. Their kidneys handled it better. Dr. Pere Gines, who led one of those studies in the Gut and Liver Journal, says strict sodium limits might actually harm patients. When you cut sodium too low, your kidneys get even more stressed. Blood flow to them drops. That raises the risk of hepatorenal syndrome-a deadly kidney failure that can happen in cirrhosis. One study showed this risk jumped from 18% to 35% in patients on ultra-low sodium diets. So now we’re stuck. Do we follow the guidelines that say <2 grams? Or do we follow the new data that says 5-6.5 grams works better?What Doctors Are Actually Doing
In practice, most hepatologists aren’t sticking to the old rules. At the 2022 AASLD meeting, 65% of liver specialists said they tailor sodium advice to each patient. Some go with 3-4 grams. Others say “don’t add salt, but don’t panic if you eat a sandwich.” It’s not about perfection. It’s about balance. The real goal? Negative sodium balance. That means your body needs to pee out more sodium than you eat. That’s where diuretics come in.
Diuretics: The Real Workhorses of Ascites Control
Medication does the heavy lifting. Sodium restriction helps, but it’s not enough on its own. Diuretics are what actually pull fluid out. The first-line drug is spironolactone. It’s a potassium-sparing diuretic that blocks the hormone aldosterone-the same one that makes your kidneys hold onto salt. Doctors start with 100 mg daily. If it’s not working after 3 days, they bump it up by 100 mg every few days, up to a max of 400 mg. Most patients need at least 200 mg. If that’s not enough, they add furosemide. This is a loop diuretic-it hits the kidneys harder. Start at 40 mg daily, max 160 mg. The combo works better than either alone. But you can’t just take these pills and hope for the best. You have to monitor.How Fast Should You Lose Weight?
The goal isn’t to lose pounds fast. It’s to lose fluid safely. If you have swelling in your legs too, you can aim for 1 kg (2.2 lbs) of weight loss per day. If you don’t have leg swelling, stick to 0.5 kg per day. Lose it faster than that, and you risk kidney damage or electrolyte crashes. You need to check your blood sodium at least twice a week when starting treatment. Too low? That’s hyponatremia. It’s common-30-40% of ascites patients have it. If your sodium drops below 120, you’re in danger. If it’s between 120 and 125, you might need to cut back on diuretics or restrict fluids. If you’re dehydrated and low on sodium? You need saline and less diuretics. It’s delicate.What to Avoid
Some medications make ascites worse. NSAIDs like ibuprofen and naproxen reduce blood flow to the kidneys. That’s bad news when your liver is already struggling. ACE inhibitors and ARBs-common blood pressure drugs-are also risky. One study showed cirrhotic patients on these drugs had 2.3 times higher risk of kidney failure. If you’re on them, talk to your doctor. Don’t stop cold turkey, but don’t assume they’re safe either.
What If Diuretics Don’t Work?
About 5-10% of patients have refractory ascites. Their fluid comes back no matter how much spironolactone or furosemide they take. That’s when you move to the next step: large-volume paracentesis. This is a procedure where a needle drains 5-10 liters of fluid from the belly in one go. It’s quick. It works. But you can’t do it every week. After draining that much fluid, you need albumin-human protein-to keep your blood pressure stable. You get 8 grams of albumin for every liter of fluid removed. That’s expensive. And it requires a hospital visit. Complications happen in 5-10% of cases: infection, bleeding, low blood pressure. There are other drugs-vaptans like tolvaptan. They block water retention. But they cost $5,000 to $7,000 per course. And you can only use them for 30 days. They’re not practical for long-term use.The Future: Personalized Treatment
We’re moving away from one-size-fits-all. The PROMETHEUS trial (NCT04567890), expected to finish in late 2025, will compare unrestricted versus restricted sodium diets in cirrhosis patients. That might finally settle the debate. In the meantime, doctors are looking at urine sodium levels. If you’re peeing out more than 78 mmol of sodium per day, you’re probably responding well to diuretics. If not, you might need higher doses-or a different approach.What You Should Do Right Now
If you have ascites:- Don’t panic about salt. Don’t obsess over reading every label.
- Avoid adding salt at the table. Skip processed foods when you can.
- Take your diuretics exactly as prescribed. Don’t skip doses.
- Check your weight every morning. Write it down.
- Call your doctor if you gain more than 1 kg in 2 days.
- Stop NSAIDs unless your liver specialist says it’s okay.
- Don’t drink alcohol. Ever.
Frank Drewery
December 18, 2025 AT 20:14I’ve seen this play out with my dad-cirrhosis, ascites, the whole deal. We thought going ultra-low sodium was the answer, but he got so weak and lost weight fast. Switching to a more moderate approach? He actually started eating again, kept more fluid out, and didn’t need paracentesis as often. It’s not about perfection-it’s about what keeps you alive and not starving.
Danielle Stewart
December 20, 2025 AT 17:59My mom’s a nurse in hepatology and she’s been telling me for years that the 2g sodium rule is outdated. Patients aren’t lab rats-they’re people who need to eat, survive, and not feel punished by their own bodies. The new data makes so much sense: if your kidneys are already screaming, don’t make them beg for salt. Let them breathe.
mary lizardo
December 22, 2025 AT 11:09It is profoundly irresponsible to suggest that sodium restriction beyond the AASLD guidelines is anything other than a dangerous deviation from evidence-based medicine. The referenced studies are small, single-center, and lack long-term outcomes. To abandon established protocols based on anecdotal trends is not clinical wisdom-it is negligence dressed as innovation.
jessica .
December 23, 2025 AT 14:10They want you to eat less salt because the pharma giants make more money off diuretics and liver transplants. Big Pharma doesn't want you to heal naturally. They want you dependent. And the FDA? Totally in bed with them. 2g? That’s a lie. Real people eat 5g. And guess what? We’re still alive. #BigPharmaLies
Ryan van Leent
December 24, 2025 AT 02:39Sajith Shams
December 24, 2025 AT 06:58Let me clarify this once and for all. The 2g sodium guideline was never meant for real-world application-it was a research target. Real clinical practice has always been 3-4g with diuretic titration. The 2021 study you mentioned? It was underpowered. The newer RCTs? They included patients with preserved renal function. You can't extrapolate that to advanced cirrhosis. Stop cherry-picking data. This is dangerous misinformation.
Adrienne Dagg
December 25, 2025 AT 13:24OMG I’m so glad someone finally said this 😭 I’ve been telling my mom to stop eating ‘low sodium’ soup and just eat real food. She was so depressed, felt like a failure for not sticking to it. Now she eats chicken, rice, and a little salt. Her belly’s smaller, she’s smiling again. Life > guidelines 🙏
Glen Arreglo
December 26, 2025 AT 19:04As someone who grew up in a household where salt was a luxury and liver disease was common, I’ve seen both extremes. My uncle died from hyponatremia after being told to eat nothing but steamed veggies and water. My aunt lived 8 years longer just by eating what her body craved-rice, lentils, a pinch of salt. Medicine isn’t one-size-fits-all. Compassion beats protocol when you’re fighting to live.
shivam seo
December 26, 2025 AT 21:59So let me get this straight-you’re telling me Australians and Americans are now more qualified to interpret hepatology guidelines than the AASLD because of two small trials? This is why Western medicine is collapsing. You ignore decades of consensus because some guy in a lab said ‘meh’. Pathetic. You people think you’re rebels but you’re just reckless.
Frank Drewery
December 28, 2025 AT 16:05Shivam, I get where you’re coming from. But the AASLD guidelines themselves say ‘individualize care’-they don’t say ‘force everyone under 2g’. My dad wasn’t rebelling-he was surviving. And the data? It’s not just two trials. It’s three RCTs across three countries showing the same pattern. Maybe the guidelines need to evolve, not just be worshipped.